Cooling and packing food
One common oversight is improper cooling of freshly cooked food. Failing to cool cooked dishes promptly can lead to rapid bacterial growth. After cooking, it’s crucial to cool food quickly and store it in shallow containers for immediate refrigeration or transportation.
Washing fruits and vegetables
Washing fruits and vegetables before cutting is essential to prevent the transfer of bacteria from the peel or rind to the flesh. After washing, store cut produce in waterproof containers or plastic wrap to ensure it cools properly before being placed in picnic coolers.
Cooler location
To maintain food safety, the placement of coolers is vital. It’s advisable to keep coolers in the passenger area of a vehicle instead of the trunk, where temperatures tend to be higher. Once at the picnic site, place the cooler in the shade and cover it with a blanket, keeping it closed until it’s time to eat.
Keep cold foods cold, hot foods hot
Cold foods should remain cold, while hot foods must stay hot to prevent bacteria and pathogens from multiplying. Ice packs and frozen gel packs are essential additions to coolers, and insulated containers with boiling water can keep foods hot until serving.
Handling food and handwashing

Thorough handwashing is crucial when handling food, especially as multiple hands are involved in preparing and serving dishes. In the absence of running water, hand sanitizers and paper towels can be used, though they are not as effective. Utensils and dishes should be plentiful to prevent cross-contamination, especially when preparing meats like poultry, fish, and beef.
Proper grilling
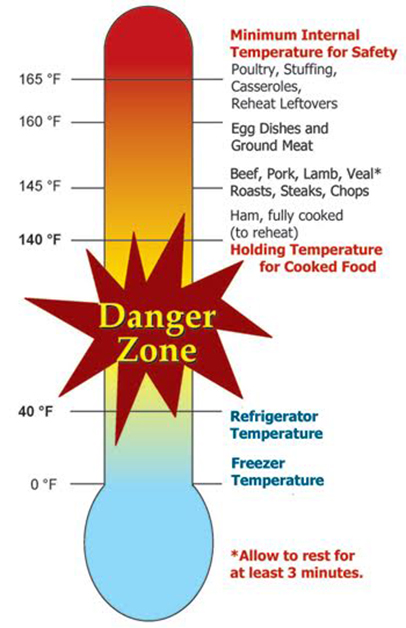
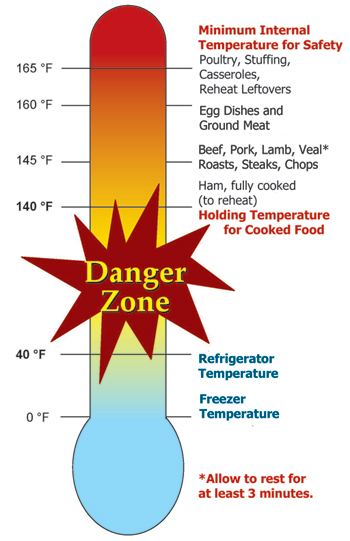
Grilling is a popular Labor Day activity, but it also poses food safety challenges. The USDA recommends three key steps for safe grilling:
- Place the Thermometer: Insert a thermometer into the thickest part of the meat to check its internal temperature.
- Read the Temperature: Wait for an accurate reading, following USDA guidelines for safe temperatures.
- Off the Grill: Remove meat and poultry from the grill once they reach their safe minimum internal temperatures, avoiding contact with raw meat or poultry.
Handling Leftovers To ensure food safety with leftovers, remember the two-hour rule: perishable items should be refrigerated within two hours (or one hour in temperatures above 90°F) to prevent bacterial growth. Use small, shallow containers for quicker cooling and freeze or consume leftovers within four days.
Reheating When reheating, cover and rotate food for even heating, especially in the microwave. Reheat sauces, soups, and gravies to a rolling boil. Slow cookers should not be used for reheating. Leftovers are safe to eat when they reach an internal temperature of 165°F.
Traveling food safety tips
For those hitting the road this Labor Day, the USDA offers the following tips to ensure food safety while traveling:
- Pack perishable foods directly from the refrigerator or freezer into the cooler.
- Use an appliance thermometer in the cooler to maintain temperatures at or below 40°F.
- Keep raw meats and poultry separate from cooked or raw foods meant to be consumed without further cooking.
- Consider using two coolers for immediate needs and perishable items.
- Choose bottled or canned drinks when camping, as untreated water from streams and rivers can be unsafe.
- Prioritize hand hygiene with hand sanitizers containing at least 60 percent alcohol.
- Think about purchasing shelf-stable food options to guarantee food safety on the go.
- While at the beach, partially bury the cooler in the sand, cover it with blankets, and use a beach umbrella for shade.
- Avoid consuming food that has been sitting out for more than two hours (or one hour in temperatures above 90°F).
By following these food safety guidelines, Americans can ensure a healthy and enjoyable Labor Day celebration, free from the risks of foodborne illnesses.
For additional food safety inquiries, individuals can contact the USDA Meat and Poultry Hotline at 888-MPHotline (888-674-6854) or chat live at ask.usda.gov from 10 a.m. to 6 p.m. EDT Monday through Friday.
(To sign up for a free subscription to Food Safety News, click here.)
]]>Oregon’s State Inspection Program meets the same regulatory safeguards that USDA requires. Before the Oregon State Inspection Program was officially sanctioned by USDA’s Food Safety and Inspection Service (FSIS), all meat for wholesale distribution had to come from federal inspection sources.
Oregon Gov. Tina Kotek said the $9 million appropriation will fund state meat inspections for the next two years. “This funding adds critical capacity for local certified meat processing to aid businesses and farm owners across Oregon,” Kotek said. “I look forward to seeing this allocation’s positive impact on Oregon’s local economy.”
The agreements are part of USDA’s commitment to supporting local and regional food systems and more resilient supply chains.
Under the cooperative agreements, the state inspection program must develop, administer, and enforce requirements “at least equal to” those implemented under the Federal Meat Inspection Act (FMIA).
USDA’s Deputy Under Secretary for Food Safety Sandra Eskin said, “This program benefits small meat and poultry processors in building their local and state marketplaces.”
USDA’s Food Safety and Inspection Service (FSIS) reached cooperative agreements with Oregon and Arkansas in 2022, under which their state inspection programs may inspect meat products produced for shipment within the state. Oregon was the 28th state to obtain FSIS approval, and Arkansas was the 29th.
FSIS has signed state inspection agreements with Arkansas Alabama, Arizona, Delaware, Georgia, Indiana, Illinois, Iowa, Kansas, Louisiana, Maine, Minnesota, Mississippi, Missouri, Montana, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, South Carolina, South Dakota, Texas, Utah, Vermont, Virginia, West Virginia, Wisconsin and Wyoming.
Lauren Henderson, acting director of Oregon’s agriculture department, says a state meat inspection program has been on her “bucket list” since the 1980s.
Oregon’s Inspection program covers the slaughter and processing of:
- Cattle
- Swine
- Sheep
- Goats
- Exotic species as defined in the rule
The slaughter and processing of poultry and rabbits are not covered at this time.
Except for custom-exempt slaughtering, the Federal Meat Inspection Act requires all amenable species, such as cattle, swine, sheep, and goats, to be slaughtered under continuous FSIS inspection.
The processing of meat and poultry products for wholesale sales is also often subject to continuous USDA inspection.
Under the new State Meat Inspection Program, businesses that operate and sell within Oregon can now sell state-inspected meat products in Oregon just like federal plants. For example, small businesses can now provide customers with inspected meat products and not rely on federally inspected plants to process the meat.
Most food processing establishments that slaughter, process, or sell meat products must have some ODA Food Safety license. Licensing does not change under the State Meat Inspection Program. Additional licensing is not required if a license already covers operations.
(To sign up for a free subscription to Food Safety News, click here.)
]]>Hurricane Idalia looms over florida
As Hurricane Idalia intensified moves through Florida and up the U.S. coast, residents are on high alert.
Tropical Storm Idalia rapidly transformed into a Category 3 hurricane. Life-threatening storm surges and dangerous winds have swept through various parts of Florida and forecasters predict it will continue up the coast.
West Virginia suffers from unrelenting flooding
As Florida prepared for Hurricane Idalia, West Virginia grappled with the aftermath of excessive rainfall, leading to widespread flooding. Gov. Jim Justice declared a State of Emergency for Kanawha, Braxton, Calhoun, Clay, and Roane counties. The torrential rains have inflicted damage upon homes, bridges, and roads in these regions.
Gov. Justice’s statement can be found here.
Ensuring food safety amidst the chaos
With both regions facing unique challenges, ensuring food safety during and after these catastrophic events remains a top priority. The U.S. Food and Drug Administration and other organizations provide crucial guidelines for residents to safeguard their food and health.
Before a storm hits:
- Elevate refrigerators and freezers off the ground using cement blocks.
- Move canned goods and foods from basements or low cabinets to higher areas.
Food safety after flooding:
- Use bottled drinking water that hasn’t come into contact with floodwater.
- Discard any food that may have been exposed to floodwater, particularly if not in waterproof containers.
- Inspect canned foods for damage, and discard damaged cans.
- Thoroughly wash and sanitize metal pans, dishes, and utensils using a chlorine bleach solution.
During power outages:
- Keep refrigerator and freezer doors closed to maintain safe temperatures.
- Use ice packs, coolers, and frozen containers of water or gel packs to preserve food freshness.
After power restoration:
- Check refrigerator and freezer temperatures; follow guidelines for safe food storage.
- Discard perishable foods that have been at temperatures above 40 degrees F for 4 hours or more.
- Refreeze frozen food if temperature remains at 40 degrees F or below.
Farmers’ concerns and resources:
- For farmers, these weather events pose serious risks to their crops. The FDA provides guidance on assessing potential damage to food crops affected by floods. If edible portions of crops are exposed to contaminated floodwaters, they’re considered adulterated and unsuitable for human consumption. Farmers are advised to evaluate the safety of crops on a case-by-case basis for potential food safety concerns.
Both West Virginia and Florida are currently marshaling resources, emergency teams, and relief efforts to aid affected residents. By following these essential food safety tips, individuals can better protect themselves and their families during these trying times. For more information, residents can access resources provided by local health departments and relevant agencies, or contact the USDA Meat and Poultry Hotline at 888-MPHotline.
Stay safe, stay informed, and stay prepared as these natural disasters unfold.
(To sign up for a free subscription to Food Safety News, click here.)
]]>The rank of countries regarding proper hand hygiene practices was: Denmark, Greece, Norway, Romania, Hungary, Germany, UK, Portugal, France, and Spain, according to a study published in the journal BMC Public Health.
Objectives were to evaluate which demographic groups are more likely to be exposed to foodborne pathogens and assess consumers’ self-reported hand hygiene practices.
Families with members aged over 65 were less likely to apply hand hygiene practices at key moments than those without elderly members. Families with children under 6 years old reported being up to twice as likely to wash their hands at critical times compared to those without kids.
“It is worrying that about half of the respondents seem to have insufficient handwashing routines to protect themselves and their family members from foodborne infection,” said researchers.
Not washing hands for long enough
Monitoring handwashing practices can be done by observation or video recording, by measuring soap consumption or in self-reported surveys. All these approaches have strengths and weaknesses, said scientists.
Questions used were part of a larger survey conducted between December 2018 and April 2019 in the European Safe Consume project.
Almost half of 7,866 respondents self-reported that they wash hands after touching raw chicken. Half of the participants washed hands with soap, however, only 15.1 percent respected the recommended duration of 20 seconds. It is advised people sing the Happy Birthday song twice to hit this time target.
High percentages of self-reported handwashing were noticed after going to the toilet and after touching something that may harbor pathogens. Only three quarters wash hands after touching raw meat or eggs.
More than half of 9,966 respondents self-reported washing hands with water and soap, as is recommended by official agencies.
Older respondents above 35 years of age were more likely to report proper hand hygiene practices than younger people. Those with a middle/high level of education were almost three times more inclined to report adequate hygiene practices at key moments, including during raw chicken preparation.
Handwashing and specific practices
The likelihood of washing hands after handling raw chicken was more than 60 percent for Danish respondents. Similar results were found for British, Greek, and Norwegian citizens.
After touching raw chicken, only 294 of 916 British respondents said they wash hands with regular soap. However, the highest frequency of washing hands for at least 20 seconds was for British respondents, while the lowest percentage was for Hungarians.
Percentages reporting handwashing after touching or feeding animals ranged from 51.3 in Denmark to 69.4 percent in Hungary.
Brits, Greeks, and Romanians were more likely to use antibacterial soap. Romanian and Greek respondents had the highest frequencies in terms of duration of handwashing.
(To sign up for a free subscription to Food Safety News, click here.)
]]>By Mitzi D. Baum, M.Sc., CEO for Stop Foodborne Illness
Stop Foodborne Illness (STOP) was born in 1994, the same year in which September was dedicated as National Food Safety Education month (NFSEM). As we quickly roll into September, I believe it’s important to reflect on the importance of both STOP and NFSEM and their contributions to public health.
STOP was formed (originally as Safe Tables Our Priority) to raise awareness and change the status quo in food safety inspection policies that were not in sync with current science. Consumers were not protected from emerging pathogens and were paying the ultimate price with their lives; four of them were children.
Through tears and pain, the parents of the children that were permanently injured or succumbed to the foodborne illnesses fought for changes in food policy that would impact everyone who eats. The first of these policy changes, in 1994, was the declaration of E. coli O157:H7 as an adulterant in ground beef. By these courageous individuals telling their horrific lived experiences brought on by food poisoning, politicians and regulatory officials made bold moves.
NFSEM is meant to educate consumers – not the food safety industry. Let’s be honest, we regularly preach to ourselves about the fundamentality of our work. NFSEM is designed to move beyond the small world of food safety professionals to engage the community at large. This is an opportunity for all food safety professionals – that work to reduce the risk of foodborne illness – to bring attention to the amazing unrecognized work performed every day in food manufacturing, retail, and food service establishments.
There is a reason that U.S. consumers assume the foods they purchase and consume are safe – it’s because of YOU. And as a community of individuals, food producers and growers, companies, regulatory agencies, and consumer advocacy groups that are focused on food safety and risk reduction, this is our collective opportunity to engage beyond those of us that are ‘in the know’.
It’s essential that the food safety community engage in the educational component of our work to the outside world. Stop Foodborne Illness sees the need for the industry to coalesce around this issue in a way that is simple, accessible, and educational while raising awareness of food safety. STOP3000 is a 30-day challenge for everyone to walk 3,000 steps each day in September to commemorate the estimated 3,000 lives lost annually in the U.S. due to food poisoning. Consider this, since 1994 over 87,000 individuals have died because of something they ate.
We, at STOP, urge you to take the challenge, sign up, raise awareness, share food safety tidbits, and support our work by participating in our third annual STOP3000. STOP operates solely on donations – we can’t do our work without the support of the food safety community. We are grateful to our sponsors this year: Chick-fil-A, Conagra Brands, Saldesia – Goddess of Food Safety, Image Base, Kelleher Consultants, LLC, and ASI Food Safety.
STOP is “The Voice for Safe Food”. This September, help us expand our voice to improve food safety and reduce the incidence of foodborne disease.
Check us out at: https://stopfoodborneillness.org/stop3000-2023/
(To sign up for a free subscription to Food Safety News,click here)
]]>Caffeinated energy drinks are beverages or mixtures that include added caffeine, often accompanied by various other ingredients like vitamins, minerals, taurine and herbal elements. These products can also contain natural caffeine sources such as guarana and yerba mate. In Canada, these drinks are allowed to have a maximum caffeine content of 180 mg per serving.
Consumers are urged to carefully review product labels to ascertain the caffeine content per serving, the number of servings in the container, and the recommended daily consumption. It is advised that CEDs should not be consumed by individuals younger than 14 years old, pregnant or breastfeeding women, or those sensitive to caffeine. Adults aged 18 and over are cautioned not to exceed a daily caffeine intake of 400 mg.
Excessive caffeine consumption can result in adverse health effects including insomnia, irritability, headaches, and nervousness. The CFIA has recently recalled certain caffeinated energy drinks because of excessive caffeine levels and improper labeling, including missing cautionary statements. Consumers are encouraged to report any consumption-related incidents to the CFIA and can also reach out to the manufacturers directly.
To ensure safety, the CFIA recommends that children, pregnant or breastfeeding individuals, and those sensitive to caffeine refrain from consuming caffeinated energy drinks. Others are advised to limit their intake and adhere to the cautionary instructions on the product labels.
(To sign up for a free subscription to Food Safety News, click here.)
]]>1. Weekly Menu Planning and Grocery Shopping
The process, as easy as 1, 2, 3, 4, begins with Weekly Menu Planning and Grocery Shopping. Parents are advised to plan their children’s lunch menus for the week ahead, researching ideas online and crafting a comprehensive shopping list. While shopping, a vital tip is to place frozen or refrigerated items in the cart last, just before reaching the cashier, to ensure they stay cold longer. Preventing cross-contamination is also emphasized, with a reminder to keep raw meat and poultry separate from other groceries and considering the use of bags to contain any potential leakage. Furthermore, perishable items must be stored in the fridge or freezer within two hours of purchase.
2. Safe Food Preparation
The second step, Safe Food Preparation, underlines the importance of thorough handwashing, an elementary yet frequently neglected practice. A recent USDA study has highlighted that 97 percent of participants failed to wash their hands correctly or at all when required. Proper hand hygiene is paramount to prevent foodborne illnesses, which can be transmitted through contaminated hands. The rule is clear: wash hands with soap and warm water for a full 20 seconds and dry them with a clean towel. Ensuring clean utensils, countertops, and cutting boards is equally imperative. Once these hygiene steps are observed, parents can proceed to prepare lunches for the week, including ready-to-eat items and boiled eggs.
3. Safe Packing
Safe Packing constitutes the third step and emphasizes the role of temperature control in maintaining food safety. Packing perishable items in an insulated lunch bag is recommended, as paper bags do not provide adequate insulation. To ensure optimal coldness, storing the insulated bag in the freezer overnight is advised. Two cold sources, such as frozen water bottles or freezer packs, are recommended to maintain temperatures below 40 degrees F until lunchtime. Hot items should be packed in insulated containers, which should be preheated with boiling water before the food is placed inside.
4. Safe Cooking
Lastly, the fourth step of Safe Cooking requires the use of food thermometers when preparing meals that require cooking, such as frozen foods. Food thermometers are essential to verify that the internal temperature of the food reaches safe levels to eliminate harmful bacteria. Different foods have different safe internal temperatures, and following manufacturer cooking instructions on frozen foods is equally crucial.
Sandra Eskin, Deputy Under Secretary for Food Safety at the U.S. Department of Agriculture (USDA), stresses the importance of prioritizing food safety during back-to-school preparations. “Because children are particularly at risk for serious foodborne illness, food safety must be at the top of the list when preparing lunches for school and field trips,” says Eskin.
By adhering to the four-step approach of meal preparation, parents can enjoy the peace of mind that comes with knowing their children’s lunches are both nutritious and secure.
(To sign up for a free subscription to Food Safety News, click here.)
]]>Food Standards Scotland (FSS) and the Food Standards Agency (FSA) issued voluntary industry guidance on glycerol in slush ice drinks after two children fell sick in Scotland in Lanarkshire in 2021 and in Edinburgh in 2022. Both required hospitalization and had symptoms consistent with glycerol intoxication.
Glycerol is an ingredient in slush ice drinks to prevent the liquid from freezing solid. It is allowed as an additive and there are no limits. Manufacturers can add as much of it as needed to achieve the desired technological function. The level of glycerol in slush ice drinks varies depending on the manufacturer and the product.
Visible warning
The guidance advises that sales of slush ice drinks containing glycerol should be accompanied by a written warning visible at point of sale that states: ‘’Product contains glycerol. Not recommended for children 4 years of age and under.’’
One concern is unlimited refills at theme and activity parks. The FSA said it was aware of a growing number of self-serve options at retail shops, convenience stores, and newsagents. Another problem is that refill offers are often unmonitored.
Manufacturers are being advised to tell retailers that they should not offer free refill promotions to children younger than 10, to prevent children being from exposed to excessive amounts of glycerol.
An FSA risk assessment found that young children may suffer from headaches and sickness caused by exposure to glycerol.
At very high levels of exposure – when several products are consumed by a child in a short space of time – glycerol intoxication could cause shock, hypoglycaemia and loss of consciousness.
Slush ice drinks can contain glycerol as a substitute for sugar to create the slush. The guidance asks businesses to only add glycerol at the minimum quantity technically necessary to achieve this effect.
Those older than 4 are considered unlikely to suffer ill effects from one slush drink. This is because the effects of glycerol are related to body weight.
Industry action
Adam Hardgrave, FSA head of additives, said while symptoms of intoxication are usually mild, it is important for parents to be aware of the risks – particularly at high levels of consumption.
“It is likely that there is under-reporting of glycerol intoxication, as parents may attribute nausea and headaches to other factors. We are grateful to those manufacturers who have already taken steps to reduce levels of glycerol, and to those who have already told us they will be adopting our new guidelines,” he said.
One company, Nichols, said it has reformulated Slush Puppie and Starslush products to remove glycerol, as they are predominantly sold in venues popular amongst young children.
The British Soft Drinks Association said members have been working with FSA on the glycerol guidance.
“Our members adhere to all current ingredient legislation including in relation to glycerol, which is authorized as an additive for use in the UK and Europe and has been used for a number of years by manufacturers of slush ice drinks in order to stop the product from freezing. We support this updated FSA communication for the benefit of consumers.”
Food crime assessment
Meanwhile, Food Standards Scotland has launched an online program which allows companies to assess their vulnerabilities to criminality.
The Food Crime Risk Profiling Tool means businesses can assess themselves against a series of statements on topics, such as how they source materials and their supply methods, before being given a report at the end which will highlight areas of good practice as well including guidance on areas they may wish to improve.
Ron McNaughton, head of the Scottish Food Crime and Incidents Unit at FSS, said prevention is the key to winning the battle against food crime.
“Food crime is serious fraud and related criminality in food supply chains. It could include adulteration, substitution or misrepresentation of origin amongst other criminal techniques. So we’ve decided to work with key stakeholders from the food industry and experts who have an interest in tackling fraud in food supply chains to develop an online, food crime risk profiling tool,” he said.
FSS will be holding several free online workshops later this year to help increase authenticity and improve food crime resilience – those who sign up to the tool will receive an invite to the sessions.
In mid-2022, the FSA also unveiled an online tool to help companies assess their vulnerability to food crime. It was developed by the National Food Crime Unit (NFCU).
(To sign up for a free subscription to Food Safety News, click here)
]]>They weren’t alone. According to AAA, international trips are on the rise this year —up more than 200 percent compared to 2022.
“Travelers are making up for lost time and willing to spend more to see the world,” said Paula Twidale, Senior Vice President of Travel at AAA.
But that doesn’t mean that caution should be thrown to the wind especially when it comes to food safety. Quite the opposite. Travelers actually need to be diligent about avoiding foods and drinks that could make them sick and ruin their overseas vacation.
Unfortunately, this young couple weren’t diligent enough. They were thrilled to be able to sample and dine on foods they didn’t ordinarily eat at home. After all, wasn’t that one of the best parts of travel — eating food grown in foreign countries and prepared by chefs in fancy restaurants or quaint sidewalk cafes. Or even buying interesting foods from sidewalk vendors or outdoor markets.
Unfortunately, they paid the price for that trust. After only several days, they came down with diarrhea, vomiting, and abdominal cramps. This left therm trapped in their hotel room. Seeing all of the sights of the city they were visiting, enjoying its night life, or even dining out weren’t in the cards for them. At least not for several days.
“Montezuma’s revenge,” said the doctor they went to, explaining that according to the Centers for Disease Control, traveler’s diarrhea affects 30 to 70 percent of travelers. And while the highest-risk destinations are in most of Asia, the Middle East, Africa, Mexico and Central and South America, it can occur anywhere.
The doctor advised them to get plenty of rest and drink a lot of clear fluids, not apple or pear fruit juice though. “You’ll be as good as new in a couple of days,” he told them. But he also gave them some food-safety advice from the Centers of of Disease Control (https://wwwnc.cdc.gov/travel/yellowbook/2024/preparing/food-and-water-precautions), which they heartily welcomed, They definitely didn’t want to get sick again.
Tips for travelers from CDC
As a starter, travelers should choose food with care and follow basic food-safety practices recommended in the United States when abroad.
°Stay away from “raw.” Raw food is especially likely to be contaminated with foodborne pathogens such as E. coli, salmonella, and Listeria. That includes raw or undercooked meat, fish, shellfish and produce, all of which can be contaminated. Foods of animal origin, including meat and eggs, should be cooked thoroughly. In general, fully cooked foods that are served hot and foods that travelers carefully prepare themselves are the safest.
In the case of dairy products, travelers should select pasteurized milk and milk products. That means steering away from unpasteurized, raw milk or cheeses made from raw milk.
°In areas where hygiene and sanitation are inadequate, or unknown, travers should avoid eating salads, uncooked vegetables, raw unpeeled fruits and unpasteurized fruit juices. Fruits that can be peeled are safest when peeled with a clean knife by the person who eats them. As healthy as fresh fruits and vegetables may be, if they’re contaminated with foodborne pathogens, they can make you sick — very sick.
°Be “water safe.” In many parts of the world, especially where water treatment sanitation and hygiene are inadequate, tap water can contain disease-causing bacteria, viruses, parasites or even chemical contaminants. Bottomline: it might not be safe to drink or use it for preparing food and drinks, making ice, cooking and even brushing teeth. And using questionable water to wash fresh produce won’t remove foodborne pathogens that might be on it.
Then, too, travelers should avoid drinking or even putting tap water into their mouths, unless they have assurances that it’s safe. Along these same lines, travelers should also avoid ice since it may have been made with contaminated tap water. In places where the safety of the tap water is questionable, travelers should opt for only unopened commercially factory-sealed water. And they should also ask that all beverages, even alcoholic drinks, be served without ice. The alcohol content of alcoholic beverages will not kill bacteria in ice made from contaminated water.
However, when served in unopened, factory-sealed cans or bottles, water, carbonated beverages, commercially prepared fruit drinks, alcoholic beverages, and pasteurized drinks generally can be considered safe. That’s also true for beverages made with water that has just been boiled — tea and coffee, for example.
When soap and water are not available, travelers should use an alcohol-based hand sanitizer containing at least 60 percent alcohol, then wash hands with soap and water as soon as possible. Hand sanitizer is not as effective as handwashing for removing some germs, like Cryptosporidium or norovirus, and does not work well when hands are visibly dirty or greasy. The Centers for Disease Control and Prevention (CDC) website Handwashing: Clean Hands Save Lives provides additional information.
About those babies. CDC says that for infants 6 months and younger, the safest way is to breastfeed exclusively. For infants on formula, parents should consider using liquid-ready-to-feed formula, which is sterile. When preparing formula from commercial power, the manufacturers instructions are usually sufficient. In addition, travelers should consider packing enough for their trip because manufacturing standards vary widely around the world.
Some tips from AAA
Dr. Kyle Staller, a gastroenterologist at Harvard-affiliated Massachusetts General Hospital, understands that the tendency to arrive somewhere new is to embrace it in all aspects.
But instead, he says, travelers should keep their food choices more in line with what they eat at home, drink plenty of clean water, and eat moderate portions.
He advises travelers to plan ahead when eating out. Check the restaurants and menus ahead of time to make sure at least one item will not only be delicious but also easy to digest. And in line with what CDC suggests for avoiding a foodborne illnesss.
In the event that you’re worried that some food where you’re going will disagree with you or you’re wary about it how safe it is to eat, pack some familiar snacks or even a meal substitute. Examples would be granola bars, nuts, trail mix or dried fruit. Whatever the case, they should be filling.
And just in case, take along a variety of over-the-counter products to counteract digestive woes while you’re traveling. Examples of this would be antacids, such as Tums for heartburn; Pepto-Bismol or Kaopectate for indigestion or diarrhea; Colace, Surfak, Metamucil, or Dulcolax for constipation; and Imodium for diarrhea. However don’t use Imodium if you also have signs of infection such as fever or blood in your stool. In that case, said Staller, go see a doctor.
Street food beware. Food from food trucks is more likely to contain harmful bacteria such as E. coli, salmonella and Listeria, especially in developing regions.
“This isn’t fun because some of the tastiest food is street food,” said Staller. “But if you indulge, know that you’re taking that risk. If you’re easily derailed by digestive issues, street food is a “no-go.”
Travelers insurance. AAA recommends that people research and purchase travel insurance since it does cover a variety of things, oftentimes foodborne illnesses.
Destinations. Go here (https://wwwnc.cdc.gov/travel/destinations/list) for a list of health-related information that travelers should know about the countries they’re planning to travel to. This would include required vaccinations, common diseases and how they’re spread (water plays a big part in this), and how to eat and drink safely.
(To sign up for a free subscription to Food Safety News,click here)
]]>No additional cases have been identified at this time.
Public Health recommends hepatitis A vaccination for patrons who consumed food or beverages from Panda Express between July 21–Aug. 4, 2023. Vaccination must be given within two weeks after exposure to be effective. Vaccination is not necessary for people who previously completed the hepatitis A vaccine series or are known to have had a past infection.
Hepatitis A vaccinations might be available through local pharmacies or physicians’ offices. In addition, Public Health will be offering free hepatitis A vaccinations to exposed persons at:
Antelope Valley Health Center
335 E Ave K 6 B
Lancaster, CA 93535
Monday, Aug. 14, 12:30 p.m. – 4:30 p.m.
Tuesday, Aug. 15 through Friday, Aug. 18, 8 a.m. – 4:30 p.m.
Most people will have protective levels of antibody after one dose of the Hepatitis A vaccine but can choose to visit their primary care provider to complete the series with a second dose 6 months after receiving their first dose.
Hepatitis A is a liver infection caused by the hepatitis A virus. Hepatitis A is highly contagious and can be spread from person-to-person through the fecal-oral route (when contaminated feces from an infected person are somehow ingested by another person during close personal contact) or by eating or drinking contaminated food or water). Most adults with acute hepatitis A will have symptoms that may include fever, fatigue, nausea, vomiting, abdominal pain, dark colored urine and jaundice (yellowing of the skin or eyes). Symptoms vary from mild to severe. There is no specific antiviral treatment. While prompt vaccination is likely to prevent infection, infection may occur in those who receive vaccination too late. Patrons who develop symptoms should call their provider and for a Hepatitis A test.
Vaccination is the best way to prevent disease. In addition, infection can be prevented by vaccination after a known exposure to a person with infectious hepatitis A. Older adults and people with weakened immune systems might benefit from receiving immune globulin (IG) in addition to hepatitis A vaccination for prevention after an exposure. For any questions about hepatitis A or the need for immune globulin, Public Health recommends that you speak to your primary care provider. If you do not have a regular provider, call 2-1-1 for assistance.
Public Health will continue monitoring all known individuals who may have been exposed to individuals ill with hepatitis A.
For more information, contact: http://publichealth.lacounty.gov/acd/diseases/hepa.htm
(To sign up for a free subscription to Food Safety News,click here)
]]>After a long string of infections required America’s poultry business to depopulate their flocks by 58.7 million birds in 2022-23, there is a welcomed break in the outbreak.
Highly pathogenic avian influenza (HPAI) last struck a commercial flock in the U.S. on April 18, 2023.
Veterinary experts told the 2023 Chicken Marketing Summit that nobody has a crystal ball to forecast what will happen. While commercial poultry is getting a break in North America, the same cannot be said for the rest of the world.
According to the World Organization for Animal Health, Sweden, Poland, Germany and Denmark have all seen recurrences this summer of Avian flu outbreaks. Some countries, including the United States, are reporting that the virus has jumped from birds to mammals.
Only some reports in New York’s live bird markets have marred the U.S. record since last April.
Commercial poultry businesses in the United States continue to invest in biosecurity measures because they are best barriers for the perimeters. Personal protection equipment is also used. The Centers for Disease Control and Prevention on Aug.9, 2023, updated its Avian flu work.
Commercial poultry is not in a high demand for vaccinations in the U.S, because of concern they might mask the the disease and slow identification.
Only one person in the U.S. has been confirmed as being infected by the bird flu, and that person fully recovered.
More than one year ago, CDC reported that a Colorado man tested positive for avian influenza A(H5) virus (H5 bird flu). The case occurred in a person who had direct exposure to poultry and was involved in culling (depopulating) poultry with presumptive H5N1 bird flu.
The CDC again reports that the current public health risk from Avian flu remains low.
The patient reported fatigue for a few days as his only symptom and has since recovered. The patient is being isolated and treated with the influenza antiviral drug.
The case did not change the human risk assessment for the general public, which CDC considers low. However, people with job-related or recreational exposures to infected birds are at higher risk of infection and should take appropriate precautions.
The CDC said detecting H5 bird flu may result from surface contamination of the nasal membrane. Still, it could not be determined, and the positive test result meets the criteria for an H5 case.
(To sign up for a free subscription to Food Safety News, click here.)
]]>People can be infected when they deliberately or accidentally eat a raw snail or slug containing the lungworm larvae or eat unwashed lettuce or other raw leafy vegetables that the slime of infected snails or slugs has contaminated.
Each of the 300+ PBS stations makes its own decision about when, where and if to air the film. It’s had good uptake in many markets, including Florida, Puerto Rico and various midwestern states. Programmers at other major stations have not yet aired the show because of the limitations of their schedules. The film’s distribution as an Accidental Host to PBS stations will continue through September 2025, and the content will undoubtedly hold up for at least that long, if not longer.
On the other hand, PBS Passport is an app available to anyone who supports their local PBS station at a basic level (usually $60/year). So whether or not their home station has already aired the show, a supporter can access the film at no additional charge through the PBS Passport streaming site.
Paznosian is an infectious disease specialist at UCLA and Food Safety News contributor. She is an expert in rat lungworm disease.
This public education approach comes after the best minds with the best science have concluded that Hawaii’s rat lungworm is not spreading beyond the state. In fact, Hawaii is the epicenter of rat lungworm disease which was first found in Asia.
According to Hawaii’s State Department of Health:
“Angiostrongyliasis, also known as neuroangiostrongyliasis or rat lungworm, is a disease that affects the brain and spinal cord. It is caused by a parasitic nematode (roundworm parasite) called Angiostrongylus cantonensis. The adult form of A. cantonensis is only found in rodents. However, infected rodents can pass larvae of the worm in their feces. Snails, slugs, and certain other animals (including freshwater shrimp, land crabs, and frogs) can become infected by ingesting this larvae; these are considered intermediate hosts. Humans can become infected with A. cantonensis if they eat (intentionally or otherwise) a raw or undercooked infected intermediate host, thereby ingesting the parasite.”
And the Hawaii Department of Health says this is what puts you at risk:
“You can get angiostrongyliasis by eating food contaminated by the larval stage of A. cantonensis worms. In Hawaii, these larval worms can be found in raw or undercooked snails or slugs. Sometimes people can become infected by eating raw produce that contains a small infected snail or slug, or part of one. It is not known for certain whether the slime left by infected snails and slugs are able to cause infection. Angiostrongyliasis is not spread person-to-person.”
With these results:
“This infection can cause a rare type of meningitis (eosinophilic meningitis).
The clinical presentation can vary. Symptoms can start with non-specific symptoms and evolve into more specific symptoms over the next following weeks. People may experience nausea, vomiting, and abdominal pain a few hours to a few days after ingestion. Symptoms can then progress to headache and other neurologic symptoms. Non-specific symptoms include fever, light sensitivity, muscle pain, fatigue, and insomnia. More specific symptoms may include constant headache, neck stiffness and pain, tingling or burning of the skin, double vision, bowel or bladder difficulties, and seizures.
Children may experience more fever, irritability, somnolence, lethargy, gastrointestinal symptoms, muscle twitching, convulsions, and extremity weakness. In addition, individuals may experience a few days to weeks of no symptoms followed by neurologic symptoms.
Although it varies from individual to individual, the symptoms usually last between two to eight weeks. Symptoms have also been reported to last for longer periods of time.
Risk in Hawaii
According to the Hawaii Health Department: “The majority of cases of rat lungworm that are identified in Hawaii have occurred on the Big Island, but cases, and infected intermediate hosts (snails and slugs), have also been identified on all of the major neighbor islands. Since the risk for infection is present statewide, the recommendations for preventing infection should be followed no matter where in the state you are.
Prevention:
To prevent angiostrongyliasis, the Hawaii Department of Health says don’t eat raw or undercooked snails or slugs, and if you handle snails or slugs, be sure to wear gloves and wash your hands. Eating raw or undercooked freshwater shrimp, land crabs and frogs may also result in infection, although, there have not been any documented cases in Hawaii.
You should thoroughly inspect and rinse produce using potable water. Leaves of leafy greens should be washed one by one under running potable water. Boil snails, freshwater prawns, crabs, and frogs for at least 3–5 minutes. Only drink potable water and do not drink from garden hoses.
Eliminating snails, slugs, and rats founds near houses and gardens might also help reduce risk exposure to A. cantonensis. Eliminating snails, slugs, and rats can be achieved through pesticide baits, traps, rodent proofing your home and sanitation.
(To sign up for a free subscription to Food Safety News, click here.)
]]>The state Legislature approved a measure this year making the sales possible, but it specifically bans the sale of unpasteurized, raw milk to wholesalers or retailers. The new law also reinforces the federal ban on the interstate sale of raw milk.
The law also makes it illegal to donate raw milk.
The sale of raw milk products such as cream, cheese or yogurt remains illegal.
Raw milk producers selling direct to consumers are exempted from other dairy, food handling or consumer protection laws.
Public health officials across the nation and most state health and agriculture departments advise that raw milk is dangerous because without pasteurization to kill bacteria and viruses it can cause severe illness. Pathogens often found in raw milk include E. coli, Salmonella and campylobacter.
The sale of raw milk under the new law does not give any liability protections if someone consumes it and becomes ill. Anyone harmed by consuming foods with microbial pathogens may have the option to take legal action to claim monetary damages for their injuries or wrongful death.
Sellers of raw milk should contact an insurance agent and legal counsel for more information on liability and liability protection, according to a statement from the state.
Raw milk has many advocates and consumers, despite the known food safety risks. The North Dakota Department of Agriculture is exempted from, and does not provide, any regulatory oversight of a raw milk facility, and does not provide any assurances for milk safety of a raw milk producer selling to the end consumer.
The state has posted a cautionary statement for consumers. “The Food and Drug Administration has posted many resources for individuals, providing factual information about raw milk and misconceptions about its purported benefits: https://www.fda.gov/food/buy-store-serve-safe-food/raw-milk-misconceptions-and-danger-raw-milk-consumption
“Pasteurized milk is a proven safe product that provides the essential nutrients of a healthy diet, without the risks associated with raw milk,” according to the statement.
The state of North Dakota has published information for raw milk sellers that includes:
- Milk is produced on dairy farms, an environment that naturally contains a plethora of microorganisms, including yeasts, molds, viruses and bacteria.
- Healthy animals can carry disease-causing germs such as e. coli O157:H7, campylobacter jejuni, and pathogenic serotypes of salmonella.
- People have also contracted tuberculosis, undulant fever and Q fever from consuming raw milk.
(To sign up for a free subscription to Food Safety News,click here)
]]>Into the cart it went. When she got home, she opened it and excitedly showed it to her husband. Does it look OK to you, she asked. He picked it up and gave it a sniff test. Looks and smells fine to me, he said. That assured her, but in the back of her mind, she wondered about what she had read about not buying cut up fruit.
At supper, she ate almost all of the fruit and declared it delicious. Her husband had a few pieces.
Late at night, she woke up feeling sick. She ran into the bathroom with what she immediately realized was a severe case of diarrhea. Worse yet, she started vomiting. While still on the toilet, she picked up the nearby trash can and started vomiting into it. Her entire system was exploding. It scared her. To make matters worse, she was experiencing painful cramps. What could it be? Was she dying?
Her husband told her not to worry, that it was nothing more than an upset stomach. The stomach flu, perhaps. But the diarrhea and vomiting wouldn’t stop. Nor would the cramps.
She wanted to call her doctor but it was late and night, and it was Saturday. Besides which she knew he was on an overseas vacation with his family.
When morning came, she was still feeling miserable but managed to get dressed and ready to walk around the corner to an urgent care facility. But diarrhea hit again and she had to turn back. But later that afternoon, she did manage to get there.
She told the medical provider that she thought it was the cut-up fruit she had eaten. But he said it would be hard to say what it was. But he did recommend the BRAT diet — bananas, rice, apples and toast. But when she got home and googled it, she found that some physicians caution that the BRAT diet does not alleviate diarrhea and can actually cause individuals to have diarrhea for longer periods, according to randomized clinical trials.
She called the grocery store where she had bought the fruit and asked to speak to the manager. He told her he had had no complaints from any customers. When she told him how sick she was and suggested he throw out all of the cut-up fruit, he told her he was too busy “to deal with this” and hung up on her.
So much for that. She was exhausted and decided to take the Urgent Care medical provider’s advice and get plenty of rest and drink a lot of fluids. She did exactly that for 2 days and began to feel better. But she felt drained, both physically and emotionally, by the entire experience.
Several days later when she called a friend and told her about how her digestive system had “exploded,” her friend told her it could have been a foodborne pathogen, perhaps E. coli, Salmonella, Listeria or norovirus. And she explained that any of these pathogens could have gotten into the package of cut up fruit in various ways. The person handling the fruit, for example, might not have washed his or her hands before cutting it up. Or perhaps the cutting board had been used for something like meat and not washed off before being used to cut up the fruit. Maybe the knife that was used to cut up the fruit hadn’t been cleaned. Or maybe the fruit, itself, had come in with pathogens on it.
Or maybe it wasn’t even the fruit.
Once again she turned to Google and quickly discovered that she probably would never know what germ had invaded her system mainly because some of the foodborne illnesses had the very symptoms she had experienced. But her friend told her the vomiting and diarrhea had been her system’s way of getting whatever the pathogen that had been in her out of her, which is why a person shouldn’t take medicine to stop the diarrhea, unless recommended by a doctor.
She was scared and confused.
Some advice about what to do
Seek medical help as soon as possible if your symptoms are severe. Examples would be dehydration, prolonged vomiting and diarrhea, stomach pains, nausea and/or a fever over 101.5 degrees F.
Food safety attorney Bill Marler said that in many cases, doctors hedge their bets and jump to the conclusion that it’s norovirus, often referred to as a “stomach bug,” and that it will usually pass. Norovirus is the leading cause of vomiting and diarrhea, and foodborne illness in the United States.
Even so, Marler said that a patient can always ask for a stool culture to be done.
“I would push for that,” he said. “It’s good practice for doctors to order them.”
He pointed out that if the “bug” that has caused the problem turns out to be a reportable foodborne disease, such as E. coli, listeria, Salmonella, norovirus, or hepatitis, then the health department can take the necessary steps to determine what caused it and then, if enough cases have been reported, issue a recall.
Marler said that’s very important because a recall can help prevent other people from becoming ill.
Marler also said that in the case of children under 5, adults over 65, or anyone whose system is immunocompromised (in cancer treatment, for example), “You can’t mess with these infections.”
According to estimates from the Centers for Disease Control and Prevention (CDC), each year 48 million people get sick from a foodborne illness, 128,000 are hospitalized and 3,000 die.
More than half of all foodborne outbreaks in the United States are associated with restaurants, delis, banquet facilities, schools, and other institutions.
Advice from the Mayo Clinic
Here’s what to do to prevent dehydration and reduce symptoms at home when you are recovering from a foodborne illness:
° Drink plenty of clear liquids: water, clear sodas and broths, gelatin and juices. But steer clear of apple and pear juices, caffeine and alcohol.
° Avoid foods such as dairy products, fatty foods, high-fiber foods or highly seasoned foods, which can make the symptoms worse.
°When you start feeling better you can go back to your normal diet.
What to do if seeking medical help
°Write down any symptoms you’re experiencing, even any that might seem unrelated to what you’re experiencing.
° Write down key personal information, which would include any international travel or recent life changes.
°Take along a list of all medications, including vitamins or supplements, that you’re taking.
°Take along a family member or friend, who will be able to help you remember what the medical provider said.
°Write down questions to ask the medical provider.
°Record any foods eaten in the past 7 days.
°Save the receipts, if possible.
°If any of the food you suspect turns out to be the problem, save some of it (if possible) in case the health department asks for a sample. But keep some of the sample.
°Use the Internet to tap into iwaspoisoned.com, which may have some information about other people near you who have gotten sick.
°Go to foodsafetynews.com or to stopfoodborneillness.org/recent-recalls to to see if there has been a recall of food you have eaten or outbreaks of the illness for which you tested positive.
Go here (https://www.cdc.gov/foodsafety/prevention.html) to learn how to prevent coming down with a foodborne illness.
(To sign up for a free subscription to Food Safety News,click here)
]]>A total of 1,923 intoxications were reported to poison control centers (CAP) during the surveillance period, between July and December. The amount is usually around 1,300 cases. Levels in 2022 were similar to those in 2019.
The monthly poisoning peak of 2022 occurred in October when more than 1,000 cases were recorded. Nearly 40 serious cases occurred, including one person needing a liver transplant and another who had kidney failure, and two people died. In 2021, 41 serious cases and four deaths were reported.
Mushroom growth varies from year to year depending on various things, including weather, according to an article in Vigil’Anses, a newsletter published by the French Agency for Food, Environmental and Occupational Health and Safety (ANSES).
Risk factors for poisoning are poor conservation, consumption of old mushrooms in poor condition, undercooked mushrooms or eating too many, and personal sensitivity, but the major risk is confusing an edible species with a toxic one.
Digging deeper into cases
A questionnaire to better understand the circumstances of intoxication was undertaken by poison control centers. It was offered to each person calling a poison control center for mushroom poisoning to assess the methods of obtaining and identifying mushrooms, plus knowledge of ANSES’s prevention messages.
Although recommendations are issued every year by ANSES, poisonings are frequently reported to poison control centers because of the consumption of raw mushrooms by young children or the use of identification applications for smartphones.
In 2022, 1,862 people were poisoned during a meal including mushrooms. The other cases include accidental ingestion by young children or vulnerable adults.
For 1,146 meals, information on the origin of mushrooms was available. More than 92 percent had been picked but some had been bought in supermarkets, markets or greengrocers or eaten in restaurants.
Picking had taken place mainly in forest areas and less frequently in a garden. A small percentage were from the roadside. Most mushrooms had been cooked before consumption but they were eaten raw in 94 meals.
Some people had tried to identify picked mushrooms before consuming them using various ways such as a book, a smartphone application, the internet or via the help of a third party such as a pharmacist or a mycologist from an association.
The most frequently identified toxic species were Satan’s (or Devil’s) bolete, yellow agarics, poisonous lepiota types or the fly agaric.
People mainly suffered from digestive symptoms including vomiting, nausea, diarrhea or abdominal pain. Neurological issues were observed in 17 percent of patients, including dizziness or headaches. Some people showed excessive sweating or a rash, as well as cardiovascular symptoms.
Wild mushroom advice
ANSES recommends that people only collect mushrooms they know as some highly toxic ones are very similar to edible species. Poisonous types can also grow where edible varieties had been picked in the past. If there is the slightest doubt, consult a specialist before consumption.
Pick only specimens in good condition and take the entire mushroom to help with identification. Do not pick mushrooms near potentially polluted sites such as roadsides and landfills.
Store mushrooms in the fridge at a maximum of 4 degrees C (39.2 degrees F), avoid all contact with other foods and consume within two days of picking. Make sure they are cooked properly – 20 to 30 minutes in a pan or 15 minutes in boiling water – and don’t eat too many in one sitting. Also, don’t give wild mushrooms to young children or use only mobile apps for identification, due to the high risk of error.
(To sign up for a free subscription to Food Safety News, click here.)
]]>The FROST Project – which stands for Fridge Recording Over Set Time – runs from August for several months. Initial results are expected by spring or early summer next year.
Temperature loggers, sent out by FSS, will be placed in a participant’s fridge and track its temperature over two weeks. Collected information will then be analyzed by the agency to help determine the average temperature of fridges in households across Scotland.
One temperature logger should be put on the top shelf and the other on the bottom shelf with people asked to record the date the trial started.
Correct fridge temperature
Participants need to fill out a questionnaire and will then be sent two temperature loggers which will automatically record the fridge’s temperature every 10 minutes. A pre-paid envelope will be provided to return the items.
It is the first time that FSS has undertaken a citizen science project. Citizen science involves the public in collecting and analyzing data for a research project.
There are an estimated 43,000 cases of foodborne illness annually in Scotland.
Dr. Emma Agnew, senior scientific adviser at FSS, said fridges can be the first line of defense in keeping food safe.
“Fridges need to be kept at a temperature between 0-5 degrees C (32-41 degrees F) but, worryingly, a quarter of people in Scotland don’t know the correct temperature it should be at. The temperature inside your fridge can vary for several different reasons, and therefore it’s important to know what temperature it’s at. Keeping food at the correct temperature will help prevent the growth of bacteria which could cause food poisoning.”
An optional step involves taking a photo of the inside of your fridge. Pictures will be anonymized for data analysis, so won’t be linked back to the taker. They will be used to get an idea of the different food products that are being stored on the different shelves of fridges across Scotland, which will help inform consumer messaging.
Current knowledge
Agnew said a pilot study of the project earlier this year found a wide range of temperatures, even from people who knew the correct range or regularly checked their fridge temperature.
“Our FSS Consumer Tracker has also highlighted that there is a high number of people using the dial within their fridge (around 30 percent) to check temperature, assuming that this is a temperature rather than a power setting, and 1 in 5 people surveyed never check their fridge temperature,” she said.
“As there are a wide variety of factors that can influence fridge temperatures, we hope that by storing the temperature loggers in two locations within the fridge and for a long period of time, that we can get an accurate reflection of fridge temperatures in households in Scotland and how this is impacted by activities such as filling the fridge after a main food shop.”
To take part, people must be over the age of 18, be currently living in Scotland and have a food fridge in the home. For more information and to register to participate, follow this link.
(To sign up for a free subscription to Food Safety News, click here.)
]]>Since July 1, three cases of Vibrio vulnificus infections have been reported to the state health department. The three patients are between 60-80 years of age.
All three patients were hospitalized and one died. One patient reported consuming raw oysters from an out-of-state establishment. Two patients reported exposure to salt or brackish water in Long Island Sound. Both patients had pre-existing open cuts or wounds or sustained new wounds during these activities which likely led to the infections.
“The identification of these severe cases, including one fatality, due to V. vulnificus is concerning,” said DPH Commissioner Manisha Juthani, MD.
“People should consider the potential risk of consuming raw oysters and exposure to salt or brackish water and take appropriate precautions. Particularly during the hottest months of the summer, bacteria are more likely to overgrow and contaminate raw shellfish. Given our current heat wave, this may be a time to exercise particular caution in what you consume.”
Vibrio vulnificus infection is an extremely rare illness. Only five cases were reported in 2020 in Connecticut, and none in 2021 and 2022. Vibrio vulnificus infections from oysters can result in severe illness, including bloodstream infections. Vibrio vulnificus can also cause wound infections when open wounds are exposed to warm salt or brackish water (mix of salt and fresh water).
People with a Vibrio vulnificus infection can get seriously ill and need intensive care or limb amputation. About one in five people with this type of infection die. People at greatest risk for illness from Vibrio vulnificus are those with weakened immune systems and the elderly.
(To sign up for a free subscription to Food Safety News,click here)
]]>The advice comes from a risk assessment by the Food Standards Agency (FSA) and Food Standards Scotland (FSS) that shows these groups are at a higher risk of severe illness from listeriosis. The risk assessment was prompted by an outbreak of Listeria infections linked to RTE cold-smoked fish.
Past advice listed smoked fish as a food of concern with the recommendation that care should be taken during pregnancy and it should only be eaten by vulnerable groups after being thoroughly cooked.
The FSA, FSS, and UK Health Security Agency (UKHSA) have been investigating the ongoing outbreak since October 2020. There have been 19 linked cases of listeriosis in England and Scotland and four people have died, this is up from the 15 cases and three deaths reported several months ago. Most patients are above 65 years old but one was a pregnant woman.
In December 2022, Lidl recalled Deluxe Oak Smoked Scottish Louch Trout and Lighthouse Bay Smoked Trout Trimmings, produced by St James Smokehouse. Product testing found Listeria monocytogenes that matched the outbreak strain but levels were below permitted limits.
Potential for serious illness
In RTE foods that can support growth of Listeria, which include smoked fish, the bacterium must not be present in 25-grams of sample when leaving production plants, or businesses must show the products will not exceed the limit of 100 Colony Forming Units per gram (CFU/g) during their shelf life.
As the risk of serious illness from listeriosis increases with age, FSA and FSS are also advising that people older than 65 should be aware of the potential danger posed by products such as smoked salmon or trout and gravlax. Neither the cold-smoking process nor refrigeration kill Listeria.
The assessment found that while the risk of contracting listeriosis in higher-risk individuals from cold-smoked fish is low, severity of illness is high. This means there is the potential for serious illness, hospitalization, and death among higher risk groups.
Uncertainties included the difficulty in estimating the infectious dose for Listeria monocytogenes and how it varies between different vulnerable groups; the long incubation period which can make attribution to a food vehicle difficult; the initial level of contamination and how it multiplies through the food chain; and consumer behavior around use-by dates and temperature abuse.
Professor Robin May, FSA chief scientific adviser, said: “Our risk assessment shows that there is still an ongoing risk to health associated with eating cold-smoked fish for specific groups of vulnerable people, including pregnant women and individuals with impaired immunity. In light of the risk assessment, we are advising that these consumers avoid ready-to-eat cold-smoked and cured fish products.”
Those with weakened immune systems are people with certain underlying conditions such as cancer, diabetes or liver and kidney disease.
Fish processing details
Cold-smoked fish such as smoked salmon or trout, and cured fish such as gravlax, have not been fully cooked during the production process to kill any Listeria that may be present. Cold-smoked fish is normally labeled as smoked fish on packaging, so processing type is unclear. RTE cold-smoked fish typically comes in thin slices, and can be eaten cold. It may also be found in sushi.
Smoked fish products that have been heat-treated during production, such as tinned smoked fish, are safe for consumption without further cooking. These products are subjected to a high temperature during processing, which is sufficient to kill Listeria.
Gauri Godbole, consultant microbiologist at UKHSA, said: “While smoked fish has a higher risk of carrying Listeria, the overall risk to the population is very low. However, some people are more likely to get a serious infection including those who are pregnant and those with weakened immune systems. The risk also increases with age. Those who are more vulnerable can be at risk of severe illness such as meningitis and life-threatening sepsis. Listeriosis in pregnancy can cause very serious illness in mothers and their babies.”
UKHSA has identified 31 patients with microbiological and epidemiological links to eight smoked fish incidents between 2015 and June 2023, with eight deaths and three pregnancy associated patients.
(To sign up for a free subscription to Food Safety News, click here.)
]]>The poll revealed 45 percent of barbecue-goers in summer were given items such as burgers, chicken and sausages but left them untouched because of the risk of food poisoning.
Safefood conducted the survey of 300 adults across Northern Ireland to shed light on barbecue cooking habits. The group safefood promotes food safety and nutrition in Northern Ireland and the Republic of Ireland.
Advice is to use a thermometer
Research discovered that two-thirds of home barbecue chefs were unaware of the correct temperature required to ensure meats were cooked and safe to eat. It also found that 5 percent of people relied on taste to check if meat was cooked.
Almost a third of people said they used a meat thermometer to measure the internal temperature of cooked barbecue meats like burgers, chicken and sausages to determine whether they are safe to eat before serving to guests.
Safefood urged home barbecue chefs to prioritize food safety this summer by using a meat thermometer and taking the guess work out of cooking by checking burgers, chicken, kebabs, and sausages should be cooked to 75 degrees C (167 degrees F). Steaks can be served more rare as harmful bacteria are usually on the outside and not in the center.
Gary Kearney, interim CEO at safefood, said: “With almost half of Northern Ireland’s barbecue-goers having been offered raw or undercooked meat, it is crucial that home barbecue chefs across Northern Ireland eliminate any guesswork and avert any potential barbecue food poisoning mishaps this summer.”
Other tips include keeping perishable food like salads, coleslaw, and quiche in the fridge until they are ready to be served. When handling raw meat and poultry, wash hands thoroughly and frequently, including before preparing salads and other ready-to-eat foods. If there are leftovers, allow food to cool before refrigerating, however, make sure to refrigerate within two hours of cooking and use any leftovers within three days.
Alex Huston, a chef, said: “Using a meat thermometer really is a game-changer. It takes the guesswork out of grilling your favorite meats and ensures it’s cooked to perfection, both in terms of taste and safety.”
Ready meal project findings
In late 2022, safefood published research on pre-prepared convenience meals and food safety risks.
A literature review highlighted limited research into consumer behavior relating to pre-prepared convenience foods. It showed that food safety knowledge varied among sociodemographic groups and that behaviors relating to storage and following use-by dates were not always in line with the guidance.
An audit survey including 266 meals indicated that some convenience foods did not comply with legislation around ingredient and allergen lists and that details provided for reheating and freezing were insufficient.
In-home observations of 50 people showed participants did not always check the use-by instructions and were unlikely to identify food safety hazards such as damaged packaging. Some participants were willing to inappropriately reheat and consume leftovers.
Interviews with 50 consumers revealed the main reasons for using pre-prepared food products are convenience and a general belief that they are safe. Problems relating to type size, the level of detail and location of instructions were identified.
Online survey participants demonstrated relatively low safe behaviors in relation to storage, preparation and use of leftovers of pre-prepared convenience foods. Older respondents had higher food safety knowledge and safer behaviors.
(To sign up for a free subscription to Food Safety News, click here.)
]]>Also, a good time to order the book – https://www.amazon.com/Poisoned-Deadly-Outbreak-Changed-Americans/dp/B0BPKKCSM3
The documentary first premiered at the Tribeca Film Festival with multiple screenings taking place between June 9th and June 17th first premiering at the SVA Theatre on June 9th. It also was shown in the author, Jeff Benedict’s, hometown, as well as Bill Marler’s, the main character of the film.
Here’s what you can expect from the documentary based on the book Poisoned by Jeff Benedict (which has an updated cover to reflect the Netflix adaptation).Netflix was first announced to be attached to develop the documentary on the 2011 book back in November 2022.
On the rerelease of the book and the new film, Benedict said: “Turning this story into a film has been a writer’s dream. Grateful to Bill and Julie Marler for trusting me with their odyssey (I didn’t expect to find a love story when I set out to write about a food borne illness outbreak),” adding, “Lucky to have worked with Ross Dinerstein and his great filmmaking team at Campfire Studios.”
The documentary comes from director Stephanie Soechtig, who has taken on the food industry with multiple documentaries, including Tapped and GMO OMG, and other subjects with titles like Under the Gun and Fed Up. For Netflix, Soechtig was behind Knock Down the House, the documentary of Bronx-born U.S. representative Alexandria Ocasio-Cortez which dropped in May 2019. Jeff Benedict serves as executive producer on the project alongside Rebecca Evans and Ross Girard with Ross M. Dinerstein and Kristin Lazure as producers. Rod Hassler serves as cinematographer on the project, and Justin Melland is the composer.
]]>Follow these guidelines to ensure the safety of your Fourth of July feast remains intact:
The Two-Hour Rule: Refrigerate all perishable items within two hours after being taken out of the oven or refrigerator. However, if the outdoor temperature exceeds 90 degrees Fahrenheit, reduce the limit to one hour. Beyond this timeframe, perishable food enters the Danger Zone, between 40 degrees and 140 degrees Fahrenheit, where bacteria can multiply rapidly. Discard any foods left out for more than two hours to avoid foodborne illnesses.
Opt for Small and Shallow Containers: When storing leftover food, use small and shallow containers in the refrigerator or freezer. This facilitates faster cooling, minimizing the time for bacterial growth.
Freeze or Consume Within Four Days: If you plan to keep leftovers for an extended period, freeze them within four days. Freezing halts the growth of most food poisoning bacteria, except Listeria and Hepatitis A. Note that the quality of frozen leftovers may decline over time, so it’s best to consume them within two to six months for optimal taste and texture. When reheating, ensure leftovers reach an internal temperature of 165 degrees Fahrenheit to eliminate any potential bacteria.
When reheating leftovers, follow these guidelines for food safety:

Microwave Reheating: Cover and rotate the food for even heating in the microwave. Arrange food items evenly in a covered microwave-safe glass or ceramic dish, and add liquid if needed. Since microwaves have cold spots, use a food thermometer to check the internal temperature in multiple places after allowing the food to rest.
Reheating sauces, soups, and gravies: Bring sauces, soups, and gravies to a rolling boil when reheating to ensure the entire mixture reaches a safe temperature.
Avoid slow cookers for reheating: Slow cookers are not suitable for reheating leftovers. Instead, choose methods like stovetop, microwave, or oven reheating, making sure the food reaches the recommended internal temperature of 165 degrees Fahrenheit.
By following these guidelines for proper food storage, reheating, and cooking, you can ensure the safety of your Fourth of July leftovers and protect yourself and your loved ones from potential foodborne illnesses. Cooking food safely and implementing proper storage practices are crucial for a delicious and safe post-Independence Day celebration.
(To sign up for a free subscription to Food Safety News, click here.)
]]>Traditionally, the Fourth of July involves outdoor gatherings with classic dishes like hamburgers, hot dogs, grilled meats, and fresh fruits. To guarantee the safety of these delectable treats, special attention needs to be paid to the significance of cleanliness and adherence to recommended guidelines.

First and foremost, washing hands before and after handling raw meat, poultry, or seafood is crucial in preventing the transfer of bacteria. Additionally, preheating the grill and scrubbing the grate thoroughly prior to cooking eliminates remnants from previous sessions, ensuring a clean cooking surface.

Grilling enthusiasts are advised to discard any marinade used for raw meat, poultry, or seafood, placing these items at a safe distance apart on the grill. It is essential to cook foods to their appropriate internal temperatures to destroy dangerous bacteria. The USDA provides specific temperature guidelines: beef, pork, lamb, and fish should reach 145 degrees F, ground meats should be cooked to 160 degrees F, and all poultry should reach 165 degrees F.
The USDA emphasizes the necessity of using a food thermometer to accurately determine if the food is safe to consume. “You can’t tell by looking at food whether it is done.” This device should be inserted into the thickest part of the meat or poultry, or through the side of burgers and thin filets of fish for precise temperature readings.
In addition to proper grilling techniques, it is essential to handle leftovers promptly. Within two hours of serving, any remaining food should be properly packed and refrigerated. However, in hot weather conditions above 90°F, the USDA advises refrigerating leftovers within one hour to prevent bacterial growth.
To ensure comprehensive food safety information, consumers can contact the USDA Meat and Poultry Hotline at 1-888-MPHotline (1-888-674-6854), where experts are available to answer questions in English or Spanish. Consumers can also seek assistance via email at [email protected] or engage in live chat at ask.usda.gov.
By following these guidelines and taking necessary precautions, individuals can contribute to a safe and enjoyable Fourth of July celebration, safeguarding the health and well-being of their loved ones.
(To sign up for a free subscription to Food Safety News, click here.)
]]>The book delves into the practices behind the scenes of the pet food industry. Entis emphasizes the importance of pet owners educating themselves about the manufacturing processes of raw, canned, and kibbled pet foods. She warns that the reality behind the appealing packaging and enticing advertising can be shocking and disillusioning.
Entis has a personal passion for pets as she shares her home with an Australian Cobberdog named Rutlands Shalom, who thrives on a home-cooked diet prepared by Entis herself.
Former global pathogen product manager George Nagle described “TOXIC” as a fantastic companion to Entis’s previous book, “Tainted.” Other reviewers expressed similar sentiments, highlighting the book’s meticulous insight and ability to hold those responsible accountable.
To provide a glimpse into the book, Entis shares an excerpt from Chapter 9, titled “Pentobarbital’s Pervasive Presence.” The excerpt recounts the story of Mark Johnson, a California cattleman whose dogs fell ill and ultimately died after consuming Gravy Train canned dog food. The tragic incident serves as a stark example of the risks associated with certain pet food products, she says.
“TOXIC” is available in digital format from major ebook retailers and can be purchased in paperback on Amazon.
About Entis: Phyllis Entis, a retired food safety microbiologist, is no stranger to writing. In addition to her work in the field, she has established herself as a mystery writer, known for the Damien Dickens Mysteries series. Her debut novel, “The Green Pearl Caper,” was selected as a Library Journal SELF-e Selection, showcasing her storytelling abilities.
“TOXIC” draws from a variety of sources, including interviews with pet owners, public records, published articles, and FDA inspection reports.
(To sign up for a free subscription to Food Safety News, click here.)
]]>CR focused on products that had concerning levels in tests five years ago. Seven of the products were ones tested in 2018; the other seven were similar to products that were previously tested but that are no longer on the market. More about how CR tests baby foods for heavy metals is available here.
To determine how many servings of each product a child could eat per day, CR’s food safety experts considered how much of that type of food kids typically eat, using data from the Centers for Disease Control and Prevention’s National Health and Nutrition Examination Survey.
Then CR assessed the risks posed by the combined exposure to arsenic, cadmium, and lead in that food. This link CR.org shows CR’s recommendations for the products tested. The findings were a spot check of the market and should not be used to draw definitive conclusions about specific brands, according to CR.
The CR findings consider that parents feed their children many foods a day. “Because heavy metals are so pervasive in foods — and because they tend to accumulate in the body — small exposures from multiple foods can add up,” says Eric Boring, PhD, a CR chemist who oversaw our testing. “And feeding your child amounts close to the daily serving limits leaves little room for exposure to heavy metals from other foods.”
Long-term intake of heavy metals may increase the risk of a variety of health and developmental problems in young children, including a lower IQ and behavioral issues, as well as ADHD, autism, and other issues.
“Early development is a really sensitive period of time,” says Maya Deyssenroth, PhD, an assistant professor of environmental health sciences at Columbia University’s Mailman School of Public Health. “Organ systems are developing and are particularly vulnerable.”
At the same time, Boring says, “While concerning, these results are no reason to panic.” He points out that the risk comes from repeated exposure over long periods of time, not from eating a food just once or even several times. An occasional serving of even one of the foods with the highest levels is generally OK,” he says. “Just remember to mix up what your kids eat.”
To sign up for a free subscription to Food Safety News, click here)
]]>USDA’s Food Safety and Inspection Service is granting inspections to two companies. It also issued instructions to its inspection program personnel (IPP) about their roles and responsibilities with regard to inspection and verification activities in establishments that harvest or process so-called cell-cultured meat or poultry food products for human food.
FSIS cited these “key points.”
- FDA and FSIS jointly oversee the production of cell-cultured meat and poultry food products and share information necessary to carry out their respective oversight responsibilities.
- Establishments that harvest cells for cell-cultured meat and poultry food products are dual jurisdiction establishments (DJE).
- Cell-cultured meat and poultry food products are subject to the same FSIS regulatory requirements and oversight authority as meat and poultry food products derived from the slaughter of amenable species.
- Labels applied to any FSIS-regulated products comprised of or containing cell-cultured meat and poultry food products are not eligible for generic approval.
As for now, USDA is allowing two California companies, Upside Foods and Good Meat, to pursue in laboratory settings the growth of meat from animal cells. USDA and FDA are partners in the regulation of lab-grown meat. FDA earlier found the products from both companies are safe to eat.
Animal cell culture technology for lab-grown meat and poultry is a production process used to produce meat and poultry food products without much slaughter activity by growing the cells of livestock or poultry in a controlled environment, such as a bioreactor, and then harvesting those cells to grow food,
If consumers warm to it, lab-grown meat and poultry could bankrupt countless farms and ranches let alone the entire production industry. But if consumers don’t like the alternatives, the fortunes invested in lab-grown products could go the way of “New Coke.” So, there is a lot at stake over whether consumers will accept meat grown in a petri dish.
At this point, consumers are not going to see much from all the lab work. Lab-grown chicken is really expensive chicken, making large-scale production unrealistic. Public availability in a couple of upscale restaurants will likely be found long before lab-grown products show up in any grocery store or Chick-Fil-A.
These attempts at lab-growth meat and poultry are reported involve more than 150 companies worldwide doing experiments on chicken, pork, lamb, fish, and beef.
The two lab-based companies that now have USDA inspection and with it, the ability to sell the food products they produce are:
- Berkeley-based Upside Foods; and
- Alameda-based Good Meat Co., with the affiliated John Biologics.
(To sign up for a free subscription to Food Safety News, click here.)
]]>USDA’s proposed rule with new regulatory requirements to better align the voluntary “Product of USA” label claim with consumer understanding of what the claim means appears to have collected a lot of support.
The recent March through June public comment period has resulted in 3,358 individual filings with support for the rule being dominant.
Posted last March, the proposed rule allows the voluntary “Product of USA” or “Made in the USA” label claim to be used on meat, poultry, and egg products only when they are derived from animals born, raised, slaughtered, and processed in the United States.
“American consumers expect that when they buy a meat product at the grocery store, the claims they see on the label mean what they say,” Agriculture Secretary Tom Vilsack said when posting the rule for comments. “These proposed changes are intended to provide consumers with accurate information to make informed purchasing decisions. Our action today affirms USDA’s commitment to ensuring accurate and truthful product labeling.”
Under the proposed rule, the “Product of USA” label claim would continue to be voluntary. It would also remain eligible for generic label approval, meaning it would not need to be pre-approved by USDA’s Food Safety and Inspection Service (FSIS) before it could be used on regulated products, but would require supporting documentation to be on file for the agency inspection personnel to verify.
The rulemaking also proposes to allow other voluntary U.S. origin claims seen on meat, poultry, and egg products sold in the marketplace. These claims would need to include a description of the package of all preparation and processing steps that occurred in the United States upon which the claim is made.
Most recently, Farm Action, the Rural Coalition, and the American Grassfed Association issued a joint public comment in support of a proposed rule from USDA’s Food Safety and Inspection Service (FSIS). The three agricultural organizations said they favor the use of the voluntary “Product of U.S.A.” label for meat products derived from animals born, raised, slaughtered, and processed in the United States.
Current policy allows the “Product of U.S.A.” label to be used on imported meat if it merely passes through a USDA-inspected plant. Farm Action’s co-founders and the American Grassfed Association filed a petition calling for reforms to this labeling system in 2018, prompting USDA to open a public comment period. FSIS referenced that petition in its announcement of the survey that preceded this proposed rule.
The comment they’ve submitted sets forth the legal foundations of the proposed rule and enumerates the benefits it would achieve on behalf of American farmers and consumers.
Reviewing decades of research into consumer attitudes toward food labels, the comment revealed that the current label use deceives consumers, whereas the proposed rule would bring the “Product of U.S.A.” label into alignment with what consumers already believe it means.
With the proposed rule, FSIS “would take a significant step toward giving consumers the information about where their food comes from that, in survey after survey, consumers have indicated they want to have,” the comment said.
USDA said the benefits of the proposed rule are particularly compelling for U.S.-based farmers. For decades, “cheap imports masquerading as domestic products” have “[undermined] the competitive position of independent ranchers and processors” and denied them market opportunities.
“The Proposed Rule would enable consumers to confidently locate meat products derived from animals bred and raised by American ranchers, slaughtered in American processing facilities, and prepared for wholesale distribution and retail consumption by American workers.”
USDA further said that by allowing consumers to act on their well-documented preference for domestic products, the resulting shift in consumer spending “could substantially enhance market opportunities for independent ranchers and processors.”
“Commenters urged FSIS to move decisively and issue a strong final rule establishing that meat, poultry, egg, and other FSIS-regulated products must be derived from animals born, raised, slaughtered, and processed in the United States to bear a ‘Product of U.S.A.’ label,” the comment concluded.
(To sign up for a free subscription to Food Safety News, click here.)
]]>A half-century ago, Colorado’s Greeley Beef Plant was the first large-scale producer of what it called “boxed beef,” with specific cuts of beet, for restaurant and grocery store customers back East.
Today, case-ready meat, retail-ready meat, or pre-packaged meat is how the industry refers to fresh meat that is processed and packaged at a central facility and delivered store-ready for the retail meat case.
While Walmart can order case-ready cuts of meat from any number of producers these days, the fact that its first wholly-owned plant is going with case-ready products is not going unnoticed.
The “boxed beef” plant will bring 600 jobs to the Olathe area. “This is great news,” said Olathe Mayor John Bacon. “We’re thrilled that Walmart chose Olathe for its innovative facility. This huge capital investment will create more jobs that will greatly benefit the City of Olathe and our entire region.”
Olathe is the county seat of Johnson County, KS. It is the fourth-most populous city in both the Kansas City metropolitan area and the state of Kansas, with a 2020 population of 141,290.
Walmart Inc. is a retail chain of large, discount, department, and grocery stores that is headquartered in Bentonville, AR. It is already a huge purchaser of case-ready beef for its 4,700 U.S. stores with Angus beef from cattle using sustainable practices among its featured products.
The new Olathe facility will add to Walmart’s ability to control its supply chain. It follows the Walmart food production facility that opened in 2018 in Fort Wayne IN. The milk production facility supplies about 500 Walmart stores with milk products under the Great Value brand. The milk comes from dairy farms in Indiana and Michigan.
(To sign up for a free subscription to Food Safety News, click here.)
]]>
The St. Louis County Department of Public Health reported the death on June 12 when it was notified by St. Claire Hospital. The man died on June 8 from an infection caused by the bacteria Vibrio vulnificus.
County officials issued a public health warning about the raw oysters, which came from “The Fruit Stand & Seafood” in Manchester, MO. Anyone who ate raw oysters from the location and has become sick should immediately seek medical attention.
Infections from the bacteria Vibrio vulnificus cause symptoms that include abdominal cramping, nausea, vomiting, fever, chills, and blisters. Anyone who ate raw oysters from the business and became sick should inform their healthcare providers that they consumed raw shellfish that may have been contaminated with Vibrio vulnificus.
“There is no evidence that the business did anything to contaminate the oysters, which likely were already contaminated when the establishment received them,” St. Louis County health officials said.
The 54-year-old man was not identified by health officials. He consumed raw oysters from The Fruit Stand & Seafood sometime during the past week.
Officials are continuing to investigate the situation. They are conducting traceback efforts to determine where the oysters came from, according to the health department.
All oysters at the business were embargoed by the health department.
Several types of vibrio bacteria can cause disease, although Vibrio vulnificus is the type that is most likely to cause severe disease, according to county health officials. Vibriosis is a very different illness from cholera, which is caused by another vibrio species, Vibrio cholerae.
Vibrio vulnificus can be found in warm, coastal waters, usually during the summer months. People typically become sick with Vibrio vulnificus by consuming raw or undercooked oysters and other shellfish. Vibrio vulnificus can also cause wound infection if someone with skin lesions swims in or is exposed to water contaminated with the bacteria. Infections caused by Vibrio vulnificus are not spread from person to person.
People infected with Vibrio vulnificus typically begin experiencing symptoms 12 to 72 hours after consuming raw or undercooked seafood, although it may take up to a week before symptoms appear. Symptoms of infection usually come on very quickly. Unlike other types of vibriosis, Vibrio vulnificus does not typically cause diarrhea, although some people do experience gastrointestinal symptoms.
Illness caused by Vibrio vulnificus can be very serious. In the United States, the mortality rate associated with Vibrio vulnificus infection is approximately one in three people infected by the bacteria, according to the health department.
Vibrio vulnificus causes more than 95 percent of seafood-related deaths in the United States. People who have chronic liver disease or abuse alcohol, as well as people who are immunocompromised, are at an increased risk of developing severe illness and should avoid eating raw or undercooked oysters and other shellfish.
(To sign up for a free subscription to Food Safety News, click here)
]]>The study, published in the Journal of Toxicology and Environmental Health, discovered that the chemicals present in sucralose can break down human DNA, posing potential risks to human health.
Sucralose’s widespread popularity has now come under scrutiny because of the potential dangers uncovered by researchers at North Carolina State University.
Epidemiological research has indicated a connection between the rise in colorectal cancers, inflammatory bowel disease and dietary choices coupled with dysbiosis, potentially suggesting an association with sucralose consumption.
The focus of the study was to investigate the toxicological and pharmacokinetic properties of sucralose-6-acetate, an impurity and structural analog found in commercially available sucralose samples.
To evaluate the genotoxicity of sucralose-6-acetate, the researchers employed several tests. The results indicated that sucralose-6-acetate is genotoxic, causing DNA strand breaks classified as clastogenic. A single daily drink sweetened with sucralose was found to contain levels of sucralose-6-acetate that surpassed the threshold of toxicological concern for genotoxicity.
The researchers also exposed human intestinal outer lining to both sucralose-6-acetate and sucralose. They conducted an RNA-seq analysis to determine the gene expression induced by these exposures. The study unveiled that sucralose-6-acetate significantly increased the expression of genes associated with inflammation, oxidative stress and cancer. Of particular note was the heightened expression of the metallothionein 1 G gene (MT1G). Moreover, both sucralose-6-acetate and sucralose impaired intestinal barrier integrity.
Further investigation demonstrated that sucralose-6-acetate inhibits two enzymes, CYP1A2 and CYP2C19, belonging to the cytochrome P450 family responsible for drug metabolism.
These findings have raised significant concerns about the safety and regulatory status of sucralose itself. Understanding the genotoxicity of sucralose-6-acetate, its potential impact on human health, and its influence on intestinal barrier integrity necessitate further exploration, according to the researchers.
The full study can be found here.
(To sign up for a free subscription to Food Safety News, click here.)
]]>Food Standards Scotland (FSS) said it was aware of two children, in Edinburgh in 2022 and Lanarkshire in 2021, who became unwell after having slush ice drinks. Both required hospitalization and had symptoms consistent with glycerol intoxication. One of the youngsters consumed three slushies in a limited time.
Glycerol is an ingredient in slush ice drinks to prevent the liquid from freezing solid. It is allowed as an additive and there are no limits. Manufacturers can add as much of it as needed to achieve the desired technological function. The level of glycerol in slush ice drinks varies depending on the manufacturer and the product.
FSS has been looking into the incident with the Food Standards Agency (FSA), Public Health Scotland, NHS Health Protection Teams, and local authorities.
Stuart McAdam, head of incidents at Food Standards Scotland, said: “Although glycerol is generally of low toxicity, there are concerns about the effect on young children when large quantities are consumed over a short period of time.
“We are working with UK trade associations that represent the soft drinks industry and a wide variety of stakeholders to better understand the levels of glycerol used across the sector.”
Unlimited refills and self-serve options
One concern is unlimited refills at theme and activity parks. The FSA said it was also aware of a growing number of self-serve options at retail shops, convenience stores, and newsagents. A particular problem is refill offers are often unmonitored. There is no legislation limiting the availability of self-service refills.
Consumption of more than one drink or large volumes in short time periods, may cause significant adverse health effects in young children, said the agency.
The advice is that children, especially those under the age of 3, should not drink more than one of these types of drinks within an hour.
Young children having one 350 mL slush ice drink could potentially suffer headaches, nausea, or vomiting. Consumption of more than one drink in a short time period could lead to more severe effects.
A European Food Safety Authority (EFSA) opinion in 2017 concluded that infants could be exposed to high enough levels to cause side effects by drinking less than one 330 mL can of a flavored drink.
Awareness of the potential risk of glycerol intoxication in children when consuming slush drinks has been raised with food businesses and local authorities. FSA has provided advice and shared a risk assessment on the additive with industry and local authorities. Work on risk management is ongoing.
(To sign up for a free subscription to Food Safety News, click here)
]]>