Editor’s note: This column was originally published by MEDPAGETODAY and is reposted here with permission.
In August 2006, Ruby Trautz of Omaha, Nebraska was the first person of several to die in a foodborne outbreak after eating uncooked baby spinach laced with E. coli 0157:H7, a pathogen that makes a deadly toxin not unlike the infamous poison ricin. Not that Trautz’s doctors knew it at the time. The truth is, when the lively 81-year old first passed bloody stool, then became uremic and seized, her doctors assumed (despite her negative test) that Trautz had a terrible case of colitis due to C. difficile.
Soon after Trautz expired, however, her son-in-law Ken Costello also suffered diarrhea and agonizing abdominal pain. His doctor diagnosed diverticulitis.
Finally, in mid-September, the multi-state outbreak linked to bagged, pre-washed Dole-brand spinach packed by California’s Natural Selection Foods made national headlines. When Costello and his wife learned this news, they quickly returned to the home they had previously shared with Trautz. Sure enough, still in the fridge was an open package of spinach eaten by the entire family that was later sent to a lab where a slurry was cultured. That specimen grew the outbreak strain.
The final toll of illness for 225 infected people residing in 27 states? Although there were only five confirmed deaths, more than half were hospitalized, and 39 suffered life-threatening hemolytic-uremic syndrome.
This leafy-green fiasco was just another milestone in the story of a hazardous microbe that still thrives in many U.S. livestock. Thirteen years earlier, after surfacing in undercooked Jack in the Box hamburgers, the same toxic bug launched the career of a leading plaintiffs’ attorney featured in a new Netflix documentary called “Poisoned: The Dirty Truth About Our Food.”
Not only has “Poisoned” won kudos for its frank depiction of a “broken system that often places profit over public health” the film has much to teach doctors about growing threats along American farm-to-fork chains plus modern loopholes and legislative inertia surrounding the safety of American food.
The Story of Bill Marler
In the world of foodborne illness and food safety, Seattle attorney Bill Marler, JD, is a hero to many people. For more about his one-of-a-kind passion and style, take a look at a 2015 story in The New Yorker that covers his present-day campaign against Salmonella. But back in 1993, when Jack in the Box fare started to sicken and kill, Marler had not yet found his calling.
Then came an SOS about 9-year-old Brianne Kiner, a desperately ill child who had already spent 40 days in a coma and 5 months in a hospital connected to wires and tubes. “She was just so vulnerable, and she just ate a fricking hamburger,” was Marler’s characteristic comment in “Poisoned.”
After meeting Brianne and forcing back tears, the 35-year-old lawyer then went to work, ultimately winning the largest personal injury pay-out ($15.6 million) awarded in his state to date. It wouldn’t restore her health, but at least it would cover care for the rest of Brianne’s life.
For Marler, lawsuit upon lawsuit then followed, some stemming from further outbreaks of E. coli 0157, others involving different foodborne perps such as Salmonella, Campylobacter, hepatitis A, and Listeria. But perhaps Marler’s proudest (non-monetary) 1990s win came when Michael Taylor, JD, then a senior lawyer at the U.S. Department of Agriculture (USDA), announced that raw ground beef contaminated with E. coli 0157 would henceforth be deemed “adulterated.”
The industry reforms that followed now mean that eating a fast-food hamburger in the U.S. poses only a fraction of the risk of fresh produce, as shown by the outbreak that killed Trautz.
“Poisoned” advances this theme by educating viewers about the proximity of massive cattle feedlots and agricultural lands in Yuma, Arizona, and California’s Central Valley, a modern recipe for disaster that periodically allows animal feces to enter irrigation canals and contaminate downstream crops like romaine lettuce. Or the blatant disregard for crowding of animals and on-site sanitation in other factory farms that fuels Salmonella-laced filth that can ultimately taint poultry and eggs.
Egregious violations have even prompted criminal prosecution. The most dramatic example? The 28-year prison sentence meted out to Stewart Parnell, former CEO of the Peanut Corporation of America, after Parnell repeatedly instructed certain employees to cover up positive Salmonella tests in 2008 to 2009. The final outcome of this wanton falsification was a multistate outbreak of Salmonella typhimurium that killed at least nine people and sickened many hundreds more who consumed a slew of peanut-containing items sold in 46 states.
A Medical Call to Action
What is more relatable than food? After all, everyone eats, and everyone occasionally suffers a foodborne illness. However, some U.S. doctors tend to discount foodborne illnesses because — despite our food supply’s many imperfections — Americans suffer fewer such incidents and related deaths than residents of most other countries. Oft-cited statistics from a seminal CDC study published in 2011 concluded that, at that time, one in six Americans — roughly 48 million people — suffered a foodborne illness each year, 128,000 were hospitalized, and 3,000 died.
These data stand in stark contrast to a WHO study published in 2015. In their first-ever analysis of the global burden of foodborne disease, the authors assessed 31 individual “hazards” and reached a final estimate of 420,000 foodborne illness deaths per year — 40% in children under 5. Not surprisingly, the study listed some risks most U.S. doctors and medical students rarely if ever consider. For example, hepatotoxic aflatoxins contaminating moldy grain, or cysticercosis — larval infection with pork tapeworm — which underlies many cases of epilepsy in low- and middle-income countries.
At the same time, a universal risk both here and abroad, is non-typhoid Salmonella, which consistently ranks as the top cause of foodborne death worldwide.
My concern is that foodborne diseases and food safety are rarely covered in medical school curricula and that even seasoned MDs often lack knowledge about changing trends, contributory factors, and the messy web of government agencies and regulations (don’t get me started about the weird jurisdictions and different mindsets of the USDA and the FDA). The list goes on.
Weaving case studies involving real people, outbreaks, and regulatory policies into continuing medical education would be one way to start (for example, do most readers even know their state’s stance on the legal sale of unpasteurized milk?). Having medical students watch “Poisoned” is another.
At the end of the day, why shouldn’t doctors and other healthcare professionals join the ranks of lobbyists, advocates, and educators around ongoing farm-to-fork reform? After all, the microbes aren’t going away anytime soon, they’re only traveling farther (and becoming more antibiotic-resistant) as our food supply grows ever more global.
About the author: Claire Panosian Dunavan, MD, is a professor of medicine and infectious diseases at the David Geffen School of Medicine at UCLA and a past-president of the American Society of Tropical Medicine and Hygiene. You can read more of her writing in the “Of Parasites and Plaguesopens” column.
(To sign up for a free subscription to Food Safety News,click here)
]]>A recent mushroom poisoning case in Massachusetts has illustrated again how people who forage mushrooms can find themselves carrying home a basket of toxins, especially if they are not well-versed in local species.
Mushroom poisoning can range from an upset stomach to death.
Common symptoms of the poisoning include vomiting, diarrhea, abdominal pain, weakness or lethargy. Illness and death can come quickly in some instances.

A 63-year-old mother and her 27-year-old son showed up at UMass Memorial Medical Center in Worcester, MA, looking ill and with signs of liver and kidney damage after consuming wild mushrooms picked in their friend’s Amherst, MA, backyard. The mother and son said the symptoms hit within hours of consuming what was later identified as a death cap mushroom.
Translating for his mother, the son said the mushrooms reminded his mother of the mushrooms she would eat in Malaysia.
With the help of an experimental drug flown in from Philadelphia, the two were stabilized, though the mother had to have a liver transplant.
A study published in the journal Mycologia, took the compiled U.S. mushroom exposures as reported by the National Poison Data System (NPDS) from 1999 to 2016 and analyzed the data from those 28 years. 133, 700 cases, 7,428 a year, of mushroom exposure, mostly by ingestion, were reported. Approximately 704, 39 a year, of the exposures resulted in major harm. Fifty-two fatalities were reported during the 16-year period, mostly from cyclopeptide-producing mushrooms ingested by older adults unintentionally. The study found that the misidentification of edible mushroom species appears to be the most common cause.
While many edible mushroom species grow wild all across the U.S., stories like this show there is risk involved because of toxic and poisonous species These toxic species include lookalikes that can cause serious illness or even death when eaten. This is why it is important that a certified mushroom expert properly identify the mushrooms.
If you’re interested in mushroom foraging and how to do it safely, contact your local mushroom foraging clubs, certification programs, university extension programs, or your State’s Department of Agriculture.
(To sign up for a free subscription to Food Safety News, click here.)
]]>Kevin came into our lives early in the morning on December 10, 1998. Our second child – our first son – immediately captured our hearts, and soon showed us just how strong he was. Only hours old when he began struggling to breathe and maintain his temperature, Kevin was rushed to intensive care. Determined to live, he fought hard, and recovered within two days, leaving doctors perplexed as what could have caused his life-threatening difficulties.
As Kevin grew, his wonderful little personality began to emerge. He was clearly very bright, spending hours studying the shapes around him and trying to mimic everything his older sister Megan could do. He had a sensitive side as well, and was very in tune to the feelings and moods of those around him. I was completely in love with him.
On Kevin’s first birthday, the moving truck arrived to pack up our home in Delaware and move us to a small town near Madison, Wisconsin, where my husband had taken a new position. We improvised by celebrating him at a restaurant, with a cupcake and a candle. He didn’t mind in the least. Laid back like his dad, Kevin took it in stride, as he did the ensuing move. By the summer of 2001, we had settled into our new life. Mike was working as an economist, I was a research biostatistician at UW-Madison, Megan was starting kindergarten, and Kevin was in the “terrible twos”– frustrated that he couldn’t do everything his big sister could. That never stopped him from trying, which often ended in messes and minor disasters. Even so, I couldn’t get mad at him when he looked at me with those twinkling blue eyes…he was just too cute!
In July, we headed off on a much-anticipated family vacation, which took us from New Jersey to Maine. Stopping along the way at Plymouth Rock, Acadia National Park, the Baseball Hall of Fame, and Niagara Falls, we visited with several old friends and relatives. It was by far the best family vacation we had ever taken. Had we known what was in store for us, we would have never come home.
On Tuesday, July 31, 2001, two weeks after returning home, Kevin awoke with a mild fever. He also had diarrhea. The following day, the diarrhea was bloody. Growing concerned, we took him to the emergency room that evening, but after a short exam, they sent us home. By the next morning, Kevin was even sicker. We went back to the hospital; this time they admitted him, treated him for dehydration and bloody stools, and ran several tests. The diagnosis came in later that afternoon: E.coli O157:H7.
On August 3rd, Kevin’s kidneys started failing; he had developed what the doctors had dreaded: Hemolytic uremic syndrome (HUS). The condition destroys platelets and blood vessels, including the very small ones in the kidneys, brain, heart, and intestines. Late that night, Kevin was transferred to UW Children’s Hospital PICU. Mike and I spent the next eight days and nights in that hospital, watching our beautiful son slip away from us with every passing hour.
It was a Saturday when Kevin received his first dialysis, a three-hour procedure during which a nurse, my husband, and two of our friends had to restrain him by holding his little arms and legs, all the while talking and singing songs to reassure him. Kevin spent the rest of that day and the next two crawling around a crib, in agony from the vicious attack on his tiny body. He vomited black bile. He became drawn, and his eyes were sunken. He looked like a malnourished third-world child. And he smelled – a horrible and overwhelming smell – a smell you could never forget. During those three horrible days, he repeatedly begged us to give him some water or juice, but the doctors said it would only make him worse, so we had to tell him no. He started asking to swim in his turtle – the baby pool in our backyard. He kept up his heart-rending pleas until we finally agreed to give him a sponge bath, and the instant that washcloth came near his mouth, he instinctively grabbed it and sucked the water out of it. It broke our hearts.
Kevin continued to decline. On Tuesday, August 7th, he was placed on a ventilator and more dialysis, this time, round-the-clock. In the hope of preventing any memory of the ordeal, the doctors sedated him heavily. Every time the medication started to wear off, though, he would try to pull the tubes out, so they were forced to put braces on his arms to restrain him. When his body began to swell, doctors inserted more tubes to drain the fluid that had accumulated in both lungs. By the end of the week, he was receiving more medications than we could count to stabilize his blood pressure and heart rate. He had received eight units of blood. A special bed had to be ordered in an effort to alleviate his pain. Despite all this, hospital staff remained optimistic, assuring us that this was the typical course of recovery for kids with HUS.
But for Kevin, all of the treatments, transfusions, and medications were not enough. On August 11th at 8:20 pm, after being resuscitated twice – and just as doctors were attempting to put him on a heart-lung machine – our beloved little boy died. He was 2 years, 8 months and 1 day old. The autopsy later showed that both Kevin’s large and small intestines had died – a condition that is 100% fatal.
In the days and weeks after Kevin’s death, we were plagued, not only by grief, but by a hundred nagging questions: how could Kevin have gone from being a healthy, vibrant toddler to being dead in just 12 days? And more importantly, how did Kevin get E. coli in the first place?
We would spend the next three years trying to find the answers to these questions. What we learned – and the difficulties we encountered – were shocking.
Since E. coli O157:H7 is a reportable infectious disease, our county public health department had been notified as soon as Kevin was diagnosed. While he lay in intensive care, health department officials had interviewed my husband and me for an hour-and-a-half. They had asked for stool samples from us and our daughter so they could determine if we, too, had contracted E. coli. We had complied, and then waited for the results of the tests, as well as the investigation they promised to conduct. Incredibly, we never heard from them again.
In early September, my mother asked me if she could follow up with the public health department. We were floored when she told us what she’d learned: my husband and daughter had also tested positive for E. coli O157:H7! Their only symptom was one loose bowel movement. Had Kevin not been sick, we wouldn’t have even given it a second thought; but you would think that with three cases of E. coli O157:H7, our local and state health departments would have launched a thorough investigation. Even though reporting regulations specify that three cases constitute an outbreak, we were told that Kevin was “an isolated case.” The health department official said they regarded Kevin as the original case, and my daughter and husband as having contracting their E. colifrom him, not from a food source. Further, he said, the chances of accurately identifying the source of Kevin’s illness were less than 5 percent.
Desperate for answers, my husband and I searched for someone knowledgeable to help us. We found a lawyer who specialized in foodborne illnesses. Given that Kevin had eaten three hamburgers in the week prior to his illness, our attorney suspected a meat contamination. In November, under the Freedom of Information Act, we requested the DNA fingerprints from the USDA for all meat recalls in 2001. It took six months, and several threats of lawsuits, to obtain that information.
In 2003, after receiving and reviewing all the documents, we discovered that the PFGE pattern (or DNA) of Kevin’s E. coli matched that of a meat recall from August 2001. The recalled meat had been produced by a subsidiary of one of America’s largest agribusinesses. A year before Kevin’s illness, that company had failed the USDA’s Salmonella test — for the second time. This is significant; under USDA’s HACCP new food inspection system, failing a Salmonella test is an indicator that other foodborne pathogens are more likely to be present. And, according to USDA regulations, plants failing the Salmonella test three times are supposed to be shut down.
Not surprisingly, that same company had also tested positive in a in December 2000 random E. coli O157:H7 test, resulting in a recall of 1.1 million pounds of ground beef. USDA performed another random E. coli O157:H7 test shortly after that. While that one was negative, a July 2001 outbreak in northern Illinois and Chicago was traced back to the same offending plant.
As a result, USDA performed a non-random test for E. coli O157:H7 on August 2, 2001, and it was positive. That result led to 25 days of USDA-industry negotiations, after which the plant finally recalled 530,000 pounds of ground beef. The PFGE pattern (or DNA) for Kevin’s E. coli matched the PFGE pattern of the recalled meat.
Unfortunately, having a PFGE match is NOT sufficient evidence to prove that a producer is responsible for a particular illness. We needed to show that Kevin had consumed the recalled meat. We knew that two of the three burgers he’d eaten the week before he became ill were made from meat purchased at the same retailer. To determine if the retailer had received its meat from the producer that had issued the recall, we would need to see the distribution records.
Again, we were in for a shock. The USDA considers those records proprietary, and would not give them to us. We were forced to ask the meat producer to provide us with its records, but the producer was unable to locate those records, so we could not determine whether the suppliers/retailers had received their meat from that producer. Not giving up, we shifted our approach, and asked the retailer to provide its records. However, as there is no law requiring retailers to share such records, they refused. After much consideration and deliberation, we felt we had no other choice; in July 2004, we filed a lawsuit so we could subpoena the producer’s and the retailers’ records. We did not do this lightly. We believe we owed it to Kevin – and to our surviving children – to find out what had happened to our son.
Despite our best efforts, we were ultimately not able to prove conclusively that the recalled meat had caused Kevin’s illness, and we dropped our lawsuit. It is hard knowing that those responsible for producing the defective product that killed our child will not be held accountable. Some people said we were interested in the money but that’s not true. We just wanted to know what happened to our child. We wanted to prevent it from happening to other people. When all is said and done, accountability fosters responsibility.
What happened to our son is a tragedy that our family lives with every day. Unfortunately, Kevin is not alone. Each year in the United States, thousands of Americans suffer and die from preventable foodborne illness.
We refused to let Kevin’s death be in vain; we do not want another family to have to suffer as ours did. Since then, we have been dedicated to preventing serious foodborne illness. In 2006, we founded the Center for Foodborne Illness Research & Prevention. CFI has made great strides towards preventing foodborne illness—locally, nationally, and globally.
(To sign up for a free subscription to Food Safety News,click here)
]]>And now nearly another decade later, Schacht may be part of yet another food illnesses outbreak.
“The funny thing is, the average for Americans is that they’re in a foodborne illness outbreak every 10 years. So, the good news is that I had one decade off,” Schacht told Food Safety News.

Harvest, a food delivery service, released a statement on June 19 recalling their “French Lentil + Leek Crumbles” after receiving customer reports of the products causing gastrointestinal issues. There has been a growing number of consumers reporting illness after eating the product over the last few weeks.
“The irony of being caught up in all of this with Daily Harvest is not lost on me. I want to be careful to say that, I’m still waiting for my lab tests. I’m still waiting on the testing of the Daily Harvest product. But I suspect, based on what I’ve heard from others, that I may be in this outbreak,” Schacht said. “Nobody with this outbreak knows anything for sure right now. And the company has not been helpful for that.”
The Seattle Native has been using Daily Harvest food service for several months. She started feeling ill sometime in May, experiencing two separate nights a week or two apart of severe gastrointestinal symptoms. Her stomach felt swollen and inflamed. “I still would continue life as best as possible. And then I would have, like, these random gastro events. They were really painful. There was one night where I was traveling for work and realized I might have to go into the ER, the pain was so severe. It was scary to be woken up by that much pain.”
Over the holiday weekend, Schacht received an email from Daily Harvest saying that they were recalling the “French Lentil + Leek Crumbles.”
“I immediately emailed them, and I said, have you guys identified what the pathogen is or what the cause of the illness is? And I got an auto response. It was the same exact email that had been sent to me before.”
Schucht tossed out the bags. “I opened up my compost and tossed the bags into the garbage.” But on Friday night, before receiving the email, she drank a smoothie from Daily Harvest. “I was like, I haven’t had enough protein for the day. I’ll have, like, a protein smoothie for dessert. So I grabbed one of their prepackaged smoothies and added protein powder and blended it and was violently ill the next day.”
“And I suspect, and I can’t know for sure, it’s my gut feeling, not to make a pun of it, that based on seeing all these other complaints online, this may not be limited to just one product. But I can’t prove that. It’s just my suspicion.”
The French Lentil + Leek Crumbles
“When you order stuff from Daily Harvest, it’s sort of like you set it and forget it and they just keep shipping you on a regular basis,” Schacht explained. “You’re living your busy life and eating through this stockpile of food in your freezer. I think I ate over two bags of it (the French Lentil + Leek Crumbles). Probably a bit more. The bags are like the volume of two to three individual chip bags.”
Schacht remembers being excited that around a month ago or two months ago Daily Harvest came out with two products called crumbles — a vegetarian protein product that can be added to your daily meals. “I’m vegetarian, I’ve been vegetarian most of my life. So, it was kind of compelling to have an additional protein item to put with my meals.”
“I think I was one of the first people to order it when it was available. Cause I just thought, oh, that sounds good to add to my meals.”
She tried different ways to cook the crumbles, but found that they never seemed to turn out as advertised. “It’s sort of like finely ground nuts and lentils and then spices and maybe onion or a little bit of vegetable mixed in. All of these are finely ground, and it has a bit of a wet texture. It’s crumbly, but also wet. I wasn’t a huge fan of it, but I’d already ordered it twice.”
“I cooked it in the pan. I also microwaved it – which I did for almost all the products I ever had from Daily Harvest. They were like, you can cook it multiple ways. It never occurred to me that they would send out this item without the ingredients already cooked. My impression was that it had gone through some kind of cooking or pasteurizing process beforehand.”
Waiting
Schacht is waiting for multiple tests to come back, both to see what the cause of the illness was and what may be in the product. “I sent in the remaining product I had. I didn’t realize, but at the very bottom back of my fridge, I had one open bag and one sealed bag of the crumbles that I had missed when I had cleared out three other bags.”
Schacht is slowly recovering from these bouts of illness. About a decade ago, she started developing reactive arthritis responses from the second of the two E.coli outbreaks she was involved in.
“It’s an inflammatory response to all that my gut had been through, so I’ve had a lot of physical pain. I worked so hard in the last decade to reduce the inflammation. And diet has been a big part of that, and a lot of physical therapy to help manage and reduce inflammation. And now, I’m seeing some signs of reactive arthritis coming back. Which has been really discomforting.”
“The last couple of years, I’ve been in a good place. I’ve put in the work to be a lot healthier. I thought I was doing something supportive of my body – given my time constraints with work and life – by getting a product like Daily Harvest.”
“For folks in the food safety world who may be reading this interview, I should tell them, ‘Hey, I double-check the products that I received. And they were all thoroughly frozen. Like hard as a rock. I wasn’t concerned about spoilage.’”
She noted that with the exception of the smoothie, she cooked the food steaming hot.
“That’s the last month and a half or so, you know, my doctor and I have been trying to figure out what’s going on with me and, until the recall notice, never put it together, that it could be this that was causing me to discomfort.”
(To sign up for a free subscription to Food Safety News, click here.)
]]>By Tami Kelley
When my daughter was pregnant with her third child, she suddenly became very sick. Her stomach was badly hurting, and she was constantly nauseous to the point of not being able to keep anything down. When she went to the emergency room, she was blown off as if she was simply exaggerating or was perhaps just looking for pain medication.
A week later, after being able to get in with her regular doctor, it was finally discovered she had a salmonella infection. Once treated for that, she got better pretty quickly, and everything appeared to be fine with her and the baby.
When it was time for her to go into the hospital for her scheduled c-section, it was discovered that the baby was in distress. She was rushed into the operating room even quicker than planned. I was with my daughter in the operating room when the baby was born. The baby was purple and not breathing. A pediatrician and many nurses gathered around her, and I watched as they worked on her and tried to get her to breathe.
She finally made a little noise, and I thought things were going to be okay. But I watched the doctor shaking her head no. I watched them intubate that tiny baby. They then rushed her out of the room. Nobody knew anything else for hours. All available doctors and nurses in that labor and delivery unit at that hospital were busy trying to save my granddaughter’s life.
She had not been getting enough oxygen for at least days before the scheduled c-section. This lack of oxygen had caused her so much distress that she had a bowel movement in the womb before birth, which then caused her to aspirate that meconium into her lungs. They were having difficulty with the intubation because the tubes kept getting filled up with the sticky meconium.
She had to be intubated three times within two hours. When we were finally told this, we were also told she was being sent to the NICU at the children’s hospital, and someone from there was on their way to transport her. Everything was a blur.
We had not even had a chance to see her except for those scary moments in the operating room. When someone from children’s hospital arrived, we were told she was being treated for a traumatic brain injury and was being cooled to help stop damage to her brain.
We were able to see her for a few minutes as they were wheeling her down the hallway in the incubator to leave to be transported to children’s hospital.
She had repeated seizures most of that night. She had to be heavily sedated and was also given plasma. My daughter was allowed to discharge from the hospital the next day so that she could be with her baby, so we were finally all able to make the trip to the children’s hospital.
When we got there, nobody was allowed to hold her. We could only put our hands into the tiny NICU bed to touch her. She was on a ventilator and still had monitors on her head to watch for seizure activity. There were wires everywhere, and we were all scared. Just a few days later, her condition was even worse. Instead of the doctors saying we were going day by day, we were now going minute by minute.
We were told if she did make it, she was expected to have a very long stay in NICU. At this point, nobody was even allowed to touch her. Nurses were instructed to do what they had to do as quickly as possible so that she had the least amount of stimulation as possible. Her bed was surrounded by curtains to keep out extra light. Her organs were starting to fail, her tiny body was bloated, and she was completely reliant on the ventilator.
Miraculously, she started improving. She was needing a little less help from the ventilator each day and was doing more of the breathing on her own. When she was nine days old, her parents finally got to hold her for the first time. She still remained in NICU for another three weeks, but everyone was surprised she was suddenly improving so much.
While going through that time in NICU, tests discovered that the lack of oxygen before and during birth caused brain damage. Doctors couldn’t tell my daughter and son-in-law what this would mean for their baby as she grew up. Basically, they were told they would just have to wait and see what she could and couldn’t do. For the first month after leaving the NICU, my daughter was extremely scared that her baby wouldn’t be able to see or hear. It appeared she was not responding to external stimuli.
When she was just 2 and a half months old, she was given a hearing test, and it was discovered she had hearing loss. She was fitted for hearing aids. As she got older, it still didn’t seem that she was responding normally to things around her. However, tests showed she could now probably hear because of the hearing aids, but she had severe developmental delays that kept her from responding accordingly for a child her age.
For the first year of her life, she was abnormally quiet. She rarely made noise and never made any of the normal baby babbling sounds. After she was a little over a year old, she finally started making some of those baby noises. She had to be held to be able to sit up, but she finally started interacting more with people.
At about 18 months old, she could sit in a chair meant for 6 month old babies, and she started showing some interest in toys. She couldn’t roll over on her own until she was close to 2 years old. Pretty quickly after that, she started learning to sit up on her own. Another MRI showed diffused brain damage, and at 2 years old, she was diagnosed with cerebral palsy. A few months after this diagnosis, she started doing her own version of “crawling” to get around.
This little girl is now almost 3 years old. She still cannot walk on her own and possibly never will. She is attempting to learn to walk with a special walker for tiny kids, but her legs are not very strong and her feet turn in when she tries. She is being fitted with special braces for her legs to help her. She is now much more verbal. Most of what she says is incomprehensible, but she is starting to learn some words. It is so adorable when she says “love you” or “thank you.”
She is always such a happy baby. She is almost always laughing. She loves her sisters, and she tries so hard to follow them and do what they are doing. She loves to give kisses. We don’t know what her life will look like going forward, but we are so thankful for her. We also know that she is very determined, and we are sure she is going to continue to fight to do as much as she possibly can.
We cannot be sure the salmonella caused any of this. We will probably never know for sure what caused it. The placenta was tested and was even sent to a hospital in another state to try to determine what happened to damage it. However, nothing unusual has been found.
Maybe it was the salmonella during her pregnancy that damaged the placenta and caused all of this. Or maybe it wasn’t. Maybe it would have just happened anyway. Even if it could be conclusively determined that it was the salmonella, it wouldn’t change anything at this point because we would have no way of knowing what caused the salmonella infection in the first place.
Was it something not cooked properly at her home? Was it on something that didn’t need to be cooked? As consumers, the majority of us blindly put a lot of faith into the government and assume there are food safety protocols in place that are assuring nothing unsafe is in our food. Meanwhile, one small event of foodborne illness can potentially change a life forever.

About the author: Tami Kelley is a student pursuing a LL.M. in Agriculture and Food Law at the University of Arkansas-Fayetteville. She received her J.D. from the University of Arkansas in 2007 and her B.S. in psychology from Arkansas State University in 2001. Tami was a stay-at-home mom for many years and returned to law after becoming an empty nester. She is planning to graduate in August and is currently exploring possible opportunities.
(To sign up for a free subscription to Food Safety News, click here)
]]>Santé publique France reports that as of 13/04/2022, 53 confirmed cases have been identified, of which 51 are linked to O26 strains, and 2 to O103 strains. For 26 other cases of HUS and STEC infections notified to Public Health France, investigations are ongoing.
These 53 cases occurred in 52 children and 1 adult, who presented symptoms between 01/18/2022 (week 3) and 03/16/2022 (week 11); for 1 adult, the date of onset of symptoms is under investigation.
These 53 cases occurred in 12 regions of metropolitan France: Hauts-de-France (11 cases), New Aquitaine (8 cases), Pays de la Loire (7 cases), Brittany (6 cases), Ile-de-France (9 cases), Auvergne-Rhône-Alpes (2 cases), Bourgogne Franche-Comté (2 cases), Grand Est (2 cases), Occitanie (2 cases), Provence-Alpes-Côte d’Azur (2 cases) and Center Val-de-Loire (1 case).
The 52 sick children are aged from 1 to 17 years with a median age of 7 years; 23 (44%) are female; 46 (88%) presented with HUS, 6 (20%) with STEC gastroenteritis. Two children died. The 2 adults are over 90 years old.
Here are several of the stories – badly translated – but, still horrible to read.
Aurélie, 34, and her husband John, 40, led “a normal family life”. Everything was turned upside down when their two sons fell seriously ill, poisoned by the E. coli bacteria via Buitoni pizzas, a brand of the food giant Nestlé. The two boys of Aurélie Micouleau and John Delpech have developed what scientists call hemolytic and uremic syndromes (HUS), which particularly affect young children. The two boys have now returned home. But the damage to the kidneys is irreversible, assures John, who put his commercial activity on hold: “No doctor is able to tell us if their condition will deteriorate in a month or in twenty years”.
“She was at death’s door. She is now locked up in her body.” The parents of Léna, 12, infected in February with E. coli bacteria after eating a pizza from the Fraîch’Up range of the Buitoni brand, testify to their ordeal. A “real nightmare” that has been going on for two months now. Then the exams show “big lesions”, “in the frontal lobe and on the back of the brain”. Léna is in a vegetative state, she no longer speaks, cannot see, and is fed by nasogastric tube. ” Today, they can’t tell us if she will make it ,” the parents worry. “Our life is broken”, they conclude at the microphone of our colleagues, moved.
Aurore and her family were infected with E. coli bacteria after eating a Buitoni pizza. Eight days later, her 19-year-old son is still suffering from worrying symptoms. Health authorities have confirmed a direct link between serious health concerns detected in some forty children and the consumption of Fraîch’Up pizzas from Buitoni. She, her husband, and her son consumed it on March 21 and all were contaminated by the bacteria after eating a Buitoni brand Fraich’Up pizza. The couple have only been sick for 48 hours but their 19-year-old son, Tristan, is still bedridden . Nausea, diarrhea, vomiting, dizziness.
This Monday, April 18, 2022, the mother of a little girl who ate a Buitoni pizza testified to the hell that her family is going through in TPMP. It has now been several days since pizzas contaminated with E.coli from the Buitoni brand have been recalled. Indeed, several of them have caused poisoning in children, including the death of two of them. Amélie, Julia’s nine-year-old mother, was able to go to Cyril Hanouna’s set to talk about all this. First, the young woman opened about her family’s descent into hell: ” She even ate two pizzas, one with cheese and one with Bolognese on February 16. It was going very well and on Tuesday 22 February, she started to be sick. She contracted a kind of gastro six days later. She had diarrhea, she had a lot of wind pain, she was nauseous but she was not vomiting. I went to the general practitioner Thursday, he told me that she probably had a big gastro (…) she gave me a treatment for a gastro”. But things got worse, she continues: ” The next morning she had a waxy complexion, it’s not like gastro, I felt that she was not well, she was on the ground. I was at the pediatric ward in St Etienne, they took care of me straight away, they did check-ups. She was immediately admitted to intensive care (…) Her condition was getting worse. When I asked if my daughter was going to die , I was told that they could not answer me”. The following Sunday, the little girl was transported by helicopter from Saint Etienne to Lyon. “On Monday she went to the block, we stayed six days in intensive care (…) we were released on March 15, she is under surveillance at home, she could not go back to school” lamented Amélie who is afraid to feed her daughter now. Moreover, this contamination could have serious consequences. Apart from the fact that the checkups are not good, Julia must see the doctor every week and do urine and blood tests. She could have sequelae like blood pressure or a kidney transplant that could show up in a few years… A heartbreaking story.
At the end of January, it’s pizza night with Chloé’s family. Her 12-year-old son Robin eats a pizza from the Fraîch’up range by Buitoni, the family’s favorite brand. Two days later, he begins to have a stomachache, becomes pale, sleeps a lot. Doctors suspect gastroenteritis. But at the end of the week, his condition worsens: he no longer eats, can no longer stand, his eyes turn yellow. Chloe then takes him to the emergency room. “When we arrived at the hospital in Lille, the pediatrician bluntly told us that his vital prognosis was engaged, tells Chloé to RMC. If within 48 hours, it affects the liver, the brain, and the heart, it’s Your life passes before you, and you wonder if your life is going to end. You imagine that he is dead and that you are going to his funeral. And you wonder if you are going to live on without him. His two kidneys had stopped, they didn’t work anymore. Within a day, it was too late. He will be sentenced to life on a salt-free diet, and he may have kidney problems later. It became an anguish permanent every night I get up to see if he’s okay.” Robin’s parents are no longer alone with their questions. They joined a Facebook group where the parents of child victims are identified. This group is that of the association “SHU T – Typical Hemolytic and Uremic Syndrome “Let’s get out of silence””. One of the mothers says that her two sons are hospitalized, one of whom is still in intensive care. Among these angry parents, Malo, the father of a 4-year-old girl, Sacha. She too found herself between life and death after eating a Buitoni pizza. She stayed in the hospital for three weeks and on dialysis for 15 days.
In Saint-Varent in the Deux-Sèvres, three children aged two and a half, nine and ten years old were very seriously ill because of the Escherichia coli bacterium. Their mother confirms that she had bought a pizza from the Buitoni brand in January. Between January 25 and February 22, the life of this family from Saint-Varent, in Deux-Sèvres turned into a nightmare. It all starts with their ten-year-old daughter showing symptoms of gastroenteritis. The doctor, after an examination of the child, concluded that he had gastroenteritis. But two days later, the child screams in pain, vomits and becomes dehydrated. Taken to the emergency room, the child will be hospitalized after her mother insisted with the doctors by explaining that her daughter does not have the habit of screaming in pain. But her condition deteriorated, her renal functions, and she was rushed to the Nantes University Hospital, in the nephrology department. She is placed on dialysis four to five hours a day, then every other day. She receives blood transfusions and opioids to ease the pain. In addition to her kidneys, her liver is affected she has pancreatitis. And then little by little his condition improves. On February 5, the youngest of the siblings is sick. She is two and a half years old. Gastroenteritis is also diagnosed. but there again, the little girl’s condition deteriorates, she vomits, staggers, dozes. Urgently transported to Nantes hospital, she convulsed, and her heart was giving out. She spent six days in intensive care with a vital prognosis. Within an hour, she could have died. My daughter almost died. The little one is very seriously affected, her kidneys hardly work anymore, her liver is affected, her heart and even her brain. She develops encephalopathy. Then her condition improved, she left intensive care for the nephrology department. On February 15, it is the nine-year-old boy who is in turn ill. Same symptoms as his sisters, he is hospitalized in Nantes in serious condition, but will recover a few days later.
Mickaël and Leslie are the parents of Bérénice, 7 years old. The little girl is in a coma after eating a frozen pizza: 75 children are currently affected by E.coli contamination. Families and other families await the conclusions of this investigation, like Mickaël and Leslie, the parents of Bérénice, 7 years old. A Buitoni pizza on Wednesday noon was Bérénice’s ritual with her mother and her big sister. One Wednesday evening, at the end of February, she experiences intestinal symptoms, such as gastroenteritis: stomach aches, diarrhea. His father, Mickaël, then takes him to the doctor the next morning. He tells the rest on franceinfo: ” The doctor sent us to the emergency room. And behind, it was the descent into hell. The kidneys no longer worked; it attacked the heart. There were two cardiac arrests, including one with one-hour cardiac massage. Bérénice is sedated, placed in a coma for twelve days now.” According to the doctors of the CHRU of Tours, Bérénice suffers from a severe form of the hemolytic and uremic syndrome, caused by this bacterium. His father now tells us about the back and forth between the hospital, the house, and the school of the big one, as well as all the steps with Public Health France to find where this bacterium comes from. ” We were contacted by Public Health France the day after our admission to the hospital. They asked us questions about our diet, where did we go to do our shopping… They are still on the ‘investigation, on the analyzes, even if they are still moving towards Buitoni pizzas. It would be a trend, but we are not sure of anything yet. “
Little Marceau, 4 and a half years old, came close to death. The child, poisoned by E.coli bacteria after eating a contaminated pizza, was finally able to be treated by doctors at Lille hospital. Extremely shocked, her mother testifies to La Dépêche of the days of anguish that the family has spent. Marceau returned to school just ten days ago with strict recommendations: not to eat salty foods. And, if he hurts himself, do not take anti-inflammatories. “He will never be able to get stung in the arm again either, breathes his mother, still tested by the seven weeks she has just spent. We must keep his veins intact for a transfusion in case he has another kidney problem. “When I arrived at Lille hospital, he greeted me, telling me that the next 72 hours were going to be decisive. That the bacteria were attacking the kidneys but that it could potentially also attack the heart and the brain. J was devastated.”
The mother of Nolan, 12, and that of Yatis, 4, who have just left the hospital. Nolan, 12, is one of these little victims. He left the hospital a few days ago after two long weeks of anguish. “He vomited almost nine days, seven times a day. We went to the doctor who thought it was gastroenteritis. But he went to intensive care for three days. He was infused, probed, transfused We are tired. Tired of following its evolution. The doctors who tell us: ‘we don’t know how long he’s going to be like this, tired’”, says his mother, Vanessa Schneider, in the video of the 8 p.m. news at the top of this article. Like Nolan and Yatis, 73 other children aged 1 to 18 were infected with E. coli bacteria. On Wednesday March 30, the health authorities established a link between some of these contaminations and frozen pizzas from the Fraîch’Up range of the Buitoni brand.
Manoé, he spent twelve days in pediatric intensive care in Nantes (Loire-Atlantique), in February. Hospitalized in Brest for three weeks, Sasha, who will soon be 5 years old, is better today, but her kidneys were no longer working after consuming Buitoni pizza in mid-February. “We go to the hospital with her child because we think she has severe gastroenteritis, and then after the analyzes we tell you that she is going to intensive care”, testifies with a heavy heart, Malo Coz, a Brestois, dad of little Sasha, almost five years old, who spent three weeks at the Morvan hospital of the Brest CHRU, from March 1.The first symptoms, as early as February 26, were stomach aches and diarrhea. It was therefore impossible to make the connection with the frozen Buitoni Fraîch’Up pizza. “The doctors told us that his kidneys were no longer working. In the operating room, he had to put a dialysis catheter. At that age, you don’t have to go through that! “, accuses Malo, whose little girl was a victim of hemolytic uremic syndrome (HUS) due to contamination by the bacterium Escherichia coli. The little Brestoise was able to leave the hospital after 15 days of dialysis and now she is better. “We came home on a very strict diet. Restrictions are easing, but there is still salt and chocolate. As she loves school, she wanted to go back as soon as possible. She begged the doctor, but she only stayed in the morning last week: she is still very tired.
(To sign up for a free subscription to Food Safety News, click here)
]]>The Tiger Brands polony listeriosis outbreak began at the start of 2017 and was officially declared over in September 2018 with 1,065 confirmed cases and at least 218 deaths.

Food contaminated with Listeria may not look or smell spoiled. Symptoms of Listeria infection can include vomiting, nausea, persistent fever, muscle aches, severe headache, and neck stiffness. Young children are particularly susceptible to the infection.
Candess Du Preez picked up her 3-year-old daughter Jordin and her cousin Riley from their crèche (preschool) where they attended school daily. On Thursdays, the children were fed polony sandwiches for their afternoon snack.
But when the children returned home, something was off. Neither Jordin or Riley ate dinner.
“The next day, they woke up as normal,” Du Preez told Food Safety News. Candess and her mother walked Jordin and Riley to the crèche. They left early as the kids were being fed breakfast.
As they walked to school, Du Preez noticed her daughter was more tired than usual. “I thought she was just being tired, and I asked, ‘Okay, are you sure you’re okay?’”
“When we got to the crèche, we just thought it was one of those days they were tired. We left them and excused ourselves like normal.”
But the day turned out to be anything but normal. By early that afternoon all of the children in the crèche had to be rushed to a nearby clinic.
“When I got there, Jordin was already on oxygen. Jordin was the only one at that point on oxygen, the others were just vomiting and lame. They were tired, and lame, and vomiting,” Du Preez said. “She was blue.”
Jordin’s parents were terrified that their daughter might die.

For the next week, her parents, Joseph and Candess Du Preez, stayed as close as possible. “We slept in the parking lot by the hospital, because we didn’t want to leave her.”
During the week that the children were quarantined, investigators came to the homes of the parents to see if they had contracted the illness there. As Seventh-Day Adventists and vegans, the Du Preez do not eat meat. The Du Preez were confident the polony connected to the national outbreak wasn’t from their home.
The investigators also searched the crèche, and there they found a piece of the polony sandwich. The polony found was the Tiger Brand’s polony implicated in South Africa’s Listeria outbreak.
Jordin was uncomfortable and couldn’t sleep without her parents. She routinely removed IVs, making it difficult for doctors to administer treatment. The Du Preezs would see their child in the morning with swollen feet. She was in intense pain from headaches and vomiting, and doctors were concerned about Jordin’s kidneys and the damage they were suffering.
“It was a terrible thing to go through. It was life and death.”
Jordin, Riley and the other children began to improve and were able to return to their homes, though treatment for their Listeriosis continued for the next month.

Jordin and her cousin Riley are eight now, but they still deal with the complications of their infection, including constant pain and headaches. Jordin needed sinus surgery to treat her sleep apnea.
Du Preez says dealing with the health issues has been emotionally and financially brutal.
When asked if she holds any resentment toward Tiger Brands, Du Preez said, “I do. I do. I do.
“They are guilty, but it’s been so many years now and we are still suffering, the children are still suffering. They are found guilty, yet they deny and deny.
“It’s been five draining years. It’s been very draining.
“Just because we went to a government hospital does not mean we are not paying. We are paying. My husband almost lost his job. He is the only breadwinner in the house.
“How many other families have been affected?” she asked.
Along with the 1,000 people affected by the Tiger Brand’s listeriosis outbreak, Jordin is represented by Richard Spoor Attorneys and is still in a legal battle with the company over damages caused by the outbreak.
Tiger Brands has been fighting the lawsuit relating to its part in the deadly outbreak. The Seattle firm of Marler Clark LLP is serving as a consultant for the case attorneys. The attorneys are representing the victims on a contingency basis.
To read more about the impact of this outbreak, please see:
- South African mother loses newborn to listeriosis in 2018 Tiger brand polony outbreak
- Tiger Brands outbreak killed young mother, leaving her twin sisters to raise her daughter
- Mother describes uncertain future for her daughter after listeriosis infection
- Uncertainty after the outbreak — ‘My niece may not know her father has died’
- Parents describe their baby’s ongoing treatment and their fears for his future
More background information about the 2017-2018 South Africa Listeria outbreak can be found here.
(To sign up for a free subscription to Food Safety News, click here)
]]>Over the course of their first eight years of marriage, South African Thenjiwe Dodo and her husband tried to have a child. In 2018, after eight years, and eight miscarriages, Thenjiwe was one month away from delivering her firstborn.

Thenjiwe was extra careful about what she ate while pregnant, knowing the fragility of the life inside her. At eight months into her pregnancy, Thenjiwe had no way of knowing that Tiger Brand polony was contaminated with Listeria.
“When I bought the polony I knew I could trust them with my life. And I knew that because I was pregnant, I needed to eat more healthy than ever,” she told Food Safety News.
The Tiger Brands polony listeriosis outbreak began at the start of 2017 and was officially declared over in September 2018 with 1,065 confirmed cases and at least 218 deaths.
Thenjiwe suffered through a terrible bout of listeriosis that left her and her child’s life in danger, At the time, she had no idea it was connected to the polony she had eaten. It wasn’t until thousands of others in South Africa became sick, and the connection was made to the polony, that Thenjiwe remembered having had the Tiger Brand product before her illness.
Though Thenjiwe recovered from her lengthy fight with listeriosis, and she gave birth. Her newborn son was severely impacted by the infection and died just 16 days after his birth.
Thenjiwe has a lot of anger toward Tiger brands.
“I do not buy anything from that brand anymore. They took away something that I was waiting for almost eight years of my life.”
Along with the 1,000 people affected by the Tiger Brand’s listeriosis outbreak, Thenjiwe is represented by Richard Spoor Attorneys and is still in a legal battle with the company over damages caused by the outbreak.
Tiger Brands has been fighting the lawsuit relating to its part in the deadly outbreak. The Seattle firm of Marler Clark LLP is serving as a consultant for the case attorneys. The attorneys are representing the victims on a contingency basis, meaning without charging them.
To read about the impact of this outbreak, please see:
More background information about the 2017-2018 South Africa Listeria outbreak can be found here.
(To sign up for a free subscription to Food Safety News, click here)
]]>Reuters reported the survivors went into Madrid’s El Prado art gallery on Tuesday and threatened to commit suicide. They were removed by security officials or left voluntarily after several hours. One of the six inside the museum was in a wheelchair.
Protestors from the group Segiumos Viviendo (We Are Still Alive) wanted a meeting with Spanish Prime Minister Pedro Sánchez and additional government funds to cover medical expenses for the victims.
The association said people feel “humiliated” and “abandoned” more than 40 years since the disease became known. They added the museum was chosen as the site for the protest because culture had helped victims cope with what had happened.
In 1981, ingestion of fraudulent olive oil led to discovery of an outbreak that was later known as toxic oil syndrome (TOS). The cause is thought to have been rapeseed cooking oil denatured with aniline and illicitly sold as olive oil.
At least 20,000 people were affected and 350 died shortly after onset of the disease with many more developing chronic illness such as liver disease. Some studies put the death toll at more than 2,000.
Patients had muscle pains, called myalgia, and very high numbers of a type of white blood cell, called eosinophilia. Women under 40 years old were more frequently and severely affected than men.
There have been a number of court cases including one that began in 1987 and ended in 1989 that convicted several people, according to the Associated Press.
(To sign up for a free subscription to Food Safety News, click here.)
]]>During this year’s national Food Safety Education Month, STOP Foodborne Illness is asking their constituents and the public at large to increase awareness about foodborne illness and the fact that an estimated 3,000 people die every year from foodborne pathogens.
STOP says that “everything we do, we do to STOP 3000 people from losing their lives from something as fundamental as eating. STOP, along with industry, regulatory agencies, and consumers is focused on changing behavior and processes to improve food safety for the greater good.”
This month in recognition of annual Food Safety Education Month efforts, the group has organized a fundraiser called STOP3000. Donors who participate in STOP3000 can double their donations, thanks to a generous $100,000 challenge grant that matches every dollar given.
What is STOP3000?
STOP3000 is:
- Taking 3000 steps a day (1.3 mi) for 30 days
- Setting a fundraising goal
- Asking friends and family to donate on behalf of Stop Foodborne Illness
You can set up a fundraising page or give to STOP3000 by visiting this web page.
.About STOP
Stop Foodborne Illness is a public health non-profit organization. Since 1994, it has focused efforts on telling the “WHY” of food safety with personal advocate stories. “We are a small but mighty team of six and work tirelessly to end illness and death due to something as basic as eating because we are all at risk of foodborne illness,” according to the group’s website.
What you’re supporting with 3,000 steps:
- Salmonella/Campylobacter petition to USDA/FSIS
STOP, partnering with the Center for Science in the Public Interest, the Consumer Federation of America, Consumer Reports, individual victims and members of the public submitted a petition to FSIS stating that it is necessary to make it illegal to sell poultry contaminated with certain pathogens to reduce the incidence of Salmonella and Campylobacter illnesses.
Currently, USDA puts its mark of inspection on poultry that is not necessarily free of Salmonella and Campylobacter known to cause human illness. In 2019, these two pathogens combined accounted for 70 percent of foodborne illnesses in the United States.
2. Recall Modernization
Stop Foodborne Illness began convening a multi-faceted group from academia, food industry, and industry associations to work with USDA and FDA to modernize the recall system in the United States. On July 13, STOP and its partners published its consumer-focused action list. The working group is in its next phase of work to research and deliver concrete action steps to FDA and USDA.
- Early Detection of Foodborne Illness Literature Review
The team at STOP has been conducting a literature review to identify factors that currently limit health care professionals from ordering stool cultures and reporting results when encountering diarrheal illnesses caused by foodborne pathogens. More than 75 published articles have been reviewed with 67 of the articles meeting the criteria for inclusion in the review. The manuscript is in the final stages of review with intent to publish.
- Dave Theno Food Safety Fellowship in partnership with Michigan State University

The Dave Theno Food Safety Fellow engages in many activities including conducting his or her own research. The exiting 2019-2021 fellow, Jaime Ragos, is leading STOP’s literature review and pending publication focused on early detection of foodborne illness. Jaime has also developed a master’s level food safety course for Michigan State University’s Online Food Safety Program that will go live this fall prior to her departure to Taiwan as a Fulbright Scholar.
- Constituent Services
The development of STOP’s new website is focused on providing resources for its constituents. The newest addition, the Navigational Map, is for those who are in crisis, post-crisis or managing the long-term effects of surviving severe foodborne disease. This extensive resource, that takes you step by step through the odyssey of foodborne illness, was created by STOP constituents based on their own experiences. A video featuring Mary Heersink, whose son Damien almost died from E. coli O157:H7, welcomes you to the page and provides visitor guidance.
STOP continues its Peer-to-Peer Mentoring program which connects survivors and family members of victims seeking to engage with another person who has had a similar, traumatic foodborne illness experience.
- H.E.A.L. (Health, Educate, Advocate, Lead)
This program is under development by STOP in conjunction with constituent advocate, Rylee Gustafson. The vision of this program is to engage young adult foodborne illness survivors to support their development of leadership and advocacy skills to increase social awareness and affect food policy reform. The underlying theme of this program is communicating to young adult survivors that they are not alone; there is a community of individuals just like them with whom they can connect and be empowered.
- STOP Speakers Bureau (Constituents)
STOP regularly receives requests for its constituent advocates to tell their stories. We are fortunate to have many constituent advocates who are willing to publicly share their experiences. Managing these requests, identifying the appropriate speaker and organizing the logistics consumes staff time. STOP asks that each requester to make a donation to STOP to cover a portion of the expenses.
- STOP Speaking Engagements (Staff and Board)
STOP is well respected within the food industry and food safety community as an advocate for consumers. Its team receives many opportunities to deliver the message of its constituent advocates and share the substance of its collaborative work with academia and government.
- General Operating Expenses
“Keeping the lights on.” - Early Detection of Foodborne Illness
In collaboration with North Carolina State University, East Carolina University, Michigan State University and University of Michigan, STOP seeks to conduct in-depth research based on the early detection of foodborne illness gaps identified through the literature review, described above, and identify solutions to reduce the incidence of severe foodborne illness.
(To sign up for a free subscription to Food Safety News, click here.)
]]>The listeriosis outbreak began at the start of 2017 and was declared over in September 2018 with 1,065 confirmed cases and 218 deaths. It was traced in March 2018 to a ready-to-eat processed meat product, similar to baloney and called polony, made at a plant in Polokwane run by Enterprise Foods, which at that time was owned by multinational Tiger Brands.
Phumzile Banze fell ill in March 2018 and had to have her first child by an emergency C-section.
“I used to pray a lot. I would say to others affected by the outbreak that they should put their hope in the hands of God because I lost hope that my son would live seeing that people were dying because of this outbreak. I was so excited to have him in my life but this outbreak didn’t allow me to have the chance to celebrate my newborn. His hair was cut off. I didn’t get to enjoy him that much for the first few days of his life.”
Sibusiso, who is now 3 years old, had to go hospital for check-ups until he was aged 1 but has since made a full recovery.
Almost lost their first child
Phumzile said she started feeling sick while pregnant.
“I had diarrhea and I used to collapse but I didn’t know it was Listeria. I had pains so I went to the local clinic but they told me the baby was not due. I went back home and stayed home a week or two before going to the hospital,” said the 24-year-old.
“When they looked they said the baby’s heartrate was beating slowly and I was about to lose the baby. So I had to rush for an emergency C-section. When he arrived, the baby went to ICU. I gave birth on March 21 then I started to see the baby after March 23. When I arrived the baby was not breathing well, the moment I gave him milk he was better but when I asked the doctors they didn’t tell me what it was.
“Luckily I found a doctor who explained to me that he had an infection in the brain. The infection was now starting to spread to the whole body. They took blood to the lab and tested it. They found it was Listeria so they had to put him on a drip for him to get antibiotics.
“For 12 days he stayed at the hospital so I used to go and visit him each and every day. I was discharged on March 23 so I didn’t get any treatment for Listeria. My son was at the hospital for the first 12 days of his life.”
The stay-at-home mum was with her family and partner, Bongani, in Gauteng, Johannesburg at the time of the incident.
“I used to crave Kota (a type of South African sandwich) and buy them a lot. One day I didn’t have money so I told my partner Bongani to come with polony and when he came back with it I used to eat it. We didn’t take it seriously about this outbreak. I had never heard of Listeria. I never used to watch the news so every time when I have craved Kota I would go and buy it because it has Russians, polony and viennas. I used to eat it by itself, a week didn’t go by without me eating Kota. Now, I don’t eat polony anymore.”
Phumzile said she doesn’t plan too much for the future but hopes to stay happy and healthy together with her family as the couple now also have a 4-month-old baby girl.
(To sign up for a free subscription to Food Safety News, click here.)
]]>Travis Knorr and his wife Aimee Knorr filed the civil case in Utah’s Third Judicial District Court in Salt Lake City on March 31, 2020, seeking compensatory damages for medical costs and other direct costs from Travis Knorr’s E. coli O103:H2 infection.
His illness was determined to be part of a nationwide outbreak that the Centers for Disease Control and Prevention said was traced to raw sprouts served by Jimmy John’s restaurants. The CDC reported 51 people as confirmed infected across 10 states. Three people were so sick they had to be admitted to hospitals, including Knorr.
Travis Knorr is a 46-year-old training director with the Utah Department of Corrections. He ate a Jimmy John’s sandwich with fresh sprouts on Feb. 21, 2020, and became ill on Feb. 26. He had severe diarrhea and had to leave work on Feb. 28. Ultimately he tested positive for E. coli.
Travis provided a stool specimen on March 3, 2020, and LabCorp reported preliminary results on March 5. His stool was confirmed positive for E. coli Shiga Toxin (STEC) by EIA testing. He eventually developed a C. difficile infection and required a fecal transplant.
In a ruling this week Judge Douglas Hogan granted the Knorrs’ motion to also seek punitive damages in addition to the compensatory damages. It is relatively rare for punitive damages to be part of a food poisoning case, according to one of the couple’s attorneys, Bill Marler.
Under Utah law punitive damages are designed to punish the plaintiff in a lawsuit for knowing disregard. They also serve as a deterrent to discourage other entities from acting in the same manner.
“It will be up to the jury to decide the damages, regular and punitive. But the judge doesn’t have to do what the jury recommends,” Marler said. “Punitive damages are usually proportionate to compensatory damages but are generally not more than 10 times the amount of compensatory damages.”
Regular damages in the Knorr case could be upwards of $250,000, but those damage amounts have not been specified by Knorr’s attorneys. A trial date has been set for February 2020.
The franchisee named as the defendant in the case is Dwight & Linford Enterprises LLC, D/B/A Jimmy John’s, a Utah corporation. The case against the franchisee illustrates one of almost 80 outbreaks linked to sprouts served by Jimmy John’s restaurants across the country going back to 1973, according to documents from Benjamin Chapman, a fresh produce expert and food pathogen researcher from North Carolina State University.
“It’s past time for Jimmy John’s to pay attention to this problem,” said Marler of the overall issues with sprouts served by the restaurants across the country. “This is about behavior over time. It’s moved from ‘gee it was a mistake’ to egregious behavior.”
The judge agreed with the Knorrs’ request to seek punitive damages, saying that “although a franchisee may have taken some actions that contribute to plaintiff’s injuries, many of those same actions can rightly be ascribed to Dwight & Linford as well.
“These include failure to take the contaminated sprouts off the menu, failure to practice good risk communication toward customers, and failure to provide adequate resources to food handlers to control the cross-contamination of sprouts,” the judge continued in his granting of the Knorr’s request to seek punitive damages.
“As to Dwight & Linford’s contention that punitive damages are not supported by the evidence, in this case, plaintiffs point to these and other actions, as well as the expert opinion of Benjamin Chapman, Ph.D., to refute this claim. . .
“Finally, plaintiffs cite Utah Code, which states that punitive damages are appropriate when the acts or omissions of the defendant are the results of ‘conduct that manifests a knowing and reckless indifference toward, or disregard of the rights of others.’ “
Editor’s note: Attorney Bill Marler is the publisher of Food Safety News.
(To sign up for a free subscription to Food Safety News, click here.)
]]>William Marsh, from Glamorgan in Wales, had symptoms including stomach cramps and diarrhea at the end of a week-long all-inclusive stay at the Riu Naiboa resort in the Dominican Republic in 2018.
His illness continued on his return to the United Kingdom, but Marsh planned on returning to work. However, the morning he was due back, he woke up and had no feeling in his legs, a sensation that spread across his body.
The 58-year-old was diagnosed with Guillain-Barré syndrome, a serious condition which can be a complication from food poisoning such as Campylobacter infection, or the flu, glandular fever, HIV and some tropical diseases.
Three years after diagnosis
Marsh was in a coma for about 10 weeks and spent seven months in hospital undergoing rehabilitation. He remains paralyzed three years on from the diagnosis. The father of three cannot walk and has been unable to return to work because of the brain injury. He requires a hoist to be lifted into a wheelchair and has weakness down his left side.
An estimated 1,300 people are affected by GBS annually in the UK. About 80 percent will recover, but between 5 percent and 10 percent die and 10 percent to 15 percent experience long term effects ranging from limited mobility to dependency on a wheelchair. In people with Guillain-Barré syndrome, the immune system attacks the nerves, damaging them and stopping signals from the brain traveling along them properly, which can cause numbness, weakness and pain in the limbs.
The holiday at Riu Naiboa was booked through TUI UK Limited to mark his 25th wedding anniversary and began in July 2018. He stayed at the resort with his wife Kathryn, 51, and their 17-year-old daughter.
Tour operator TUI UK has denied liability and lawyers at Irwin Mitchell are preparing to launch court proceedings after being told to investigate in May 2020.
Impact of illness
“Kathryn, and my daughter, fell ill first and then it hit me. The symptoms were awful but we just tried to keep on going as I as I was due to go back to work,” said Marsh.
“I need so much help to do even the simplest of tasks now. I became a lot more reliant on Kathryn for help. Rather than being my wife she is now more my carer. It’s incredibly difficult to put into words how life has changed over the last few years. It is still hard to believe everything that has happened to me and it has been tough facing up to the fact that I may never walk properly again.
“Before my illness I’d never heard of Guillain-Barré but sadly I know now how dangerous it is. Throughout my time battling with Guillain-Barré syndrome, it has become clear just how misunderstood the condition is and how many people do not know much about it at all. I remain determined to get to the bottom of the cause of my illness but also to raise awareness of the support available.”
Action for Brain Injury Week runs from May 17 to 23 and is supported by the charity Headway. Marsh has also been helped by the charity Guillain-Barré and Associated Inflammatory Neuropathies (GAIN). May is GBS Awareness Month.
Jatinder Paul, a senior associate solicitor at Irwin Mitchell, said the family’s life has been turned upside down by the condition.
“What was meant to be a celebration for William and Kathryn has turned to despair with William still greatly impacted by his illness. William still has many questions about how he fell ill. We’re determined to help him establish what happened and also secure him access to the specialist support he needs to ensure he gets the best from life.”
(To sign up for a free subscription to Food Safety News, click here.)
]]>Meshack Mahlngu fell ill in late 2017 during South Africa’s Listeria outbreak — a week before he was scheduled to take his exams.
Mahlngu said the experience was “really mentally straining” as he was focused on his final exams. In South Africa, matriculation, also known as matric, is the final year of high school and the qualification received on graduating.
Impact on studies
“My situation was I contracted the disease while I was in the final year of school. I had it a week before I was taking my exams so spent the first month of them at hospital while I was diagnosed with listeriosis,” he told Food Safety News.
“I took my exams, I wrote my first two papers in the hospital and managed to go back to school when I was discharged. I got the average result, to say I passed, but for the student I was I didn’t get the results I was expecting and could have done better.
“Through the time in school I didn’t have it easy up to that point but wouldn’t say it really affected me that much because I still tried to put myself in therapy and I’m trying to cope with things that I understand. I was in hospital for post-traumatic stress disorder (PTSD) linked to the incident, as it was scary, I was still in school. There was some trauma after my illness but I’m physically OK now.”
Mahlngu lives in Johannesburg with his mum and has two younger sisters — one aged 15 and the other is 11.
“I was in the hospital for more than a month. My mum visited more than anyone, she was the one going through with all the experts when they gave me care and the expenses were doubling every time. I had never heard of Listeria or had food poisoning until I contracted the disease,” he said.
“There was a guy I knew a lot, he was a childhood friend from school and he died from listeriosis. He was a few years older than me at that time, he was 20 and I was 17.”
The now 21-year-old remembers being in church in August 2017 when he started to feel unwell.
“On Sunday at church I had a headache and the next day at school it became a severe headache and it continued the day after and then at night on the third day I decided to go to hospital. I was supposed to call an ambulance but managed to go there with my father. When we got there I was still having the headache and I got to the emergency room and was diagnosed there.”
College plans
The 2017 and 2018 listeriosis outbreak in South Africa was linked to ready-to-eat (RTE) meat products and caused more than 1,050 illnesses and at least 218 deaths.
It was traced in March 2018 to a RTE processed meat product called polony, which is similar to boloney, made at a factory in Polokwane run by Enterprise Foods, then-owned by Tiger Brands. In August 2020, Tiger Brands agreed to sell its processed meats division, which includes Enterprise Foods.
Mahlngu used to eat polony all the time at school and at home but now avoids it.
“I try to avoid a lot of products that are related to the ones that faced listeriosis, not because of Tiger Brands per se, just for health purposes. I believe they have made the correct arrangements to solve the mistakes they had that year. Mistakes happen, life is life, but I would appreciate an apology from them to the community of its customers. It wasn’t on purpose, they were not trying to kill us.”
The future for Mahlngu includes finishing a financial accounting course.
“I did my first year when I turned 18. I have two years left to finish the course. I am on hold due to financial difficulties but definitely want to finish it, that is my main goal right now,” he said.
“My future holds a lot of brightness and joy. I have a lot of plans that I believe will come true. I am pending on the college degree in financial accounting, if I can finish it that will be one of my short term goals.”
(To sign up for a free subscription to Food Safety News, click here.)
]]>Joseph Kadango, who lives in Johannesburg, spent months in hospital after becoming infected, lost his job and couldn’t support his family.
He used to buy meat such as Russians, Viennas, chicken and polony for breakfast while shopping.
“After a month they stopped and said we don’t sell that stuff anymore here and it is at that time the listeriosis started for me. They said bring it back but I couldn’t take these things back as I had eaten most of them already. I took all the polony, viennas and Russians of Enterprise and threw them in the dustbin,” he told Food Safety News.
“When I was in hospital I told my brother you must avoid those things in the bin. It is no good to eat. Now I don’t eat polony, Russians or viennas but some other people buy it. I don’t have that stuff anymore, I am afraid to eat it.”
Months in hospital
After feeling sick for a few days, the 44 year old went to see a doctor.
“I thought something was wrong and I started to feel unwell with flu symptoms and then after two days I still had a headache and feeling dizzy so I was not feeling very well. When I went to the doctor’s they said I was not OK and it was some disease. They checked me, gave me an X-ray and saw something and said it was listeriosis from something I ate. They asked me what I ate all the time. I was vomiting, my head was paining, my brain was confused and I was just like a child,” said Kadango.
“I was in hospital for three months and after that they checked me and gave me an injection. I was vomiting too much and not eating. They did something to my spinal cord to drain fluid. Now I am feeling well and getting better, it is not like before when it was very bad.”
The 2017 and 2018 listeriosis outbreak in South Africa was linked to ready-to-eat (RTE) meat products and caused more than 1,050 illnesses and at least 218 deaths.
It was traced in March 2018 to a RTE processed meat product called polony made at a factory in Polokwane run by Enterprise Foods, then-owned by Tiger Brands. In August 2020, Tiger Brands agreed to sell its processed meats division, which includes Enterprise Foods.
No one to support the family
Kadango is now unemployed. He had a business selling items including clothes and shoes before getting ill. He lives at home with three younger brothers and his child, a 16-year-old boy.
“At that time I was working and my business was going well but when I was sick everything started to get complicated with my child going to school,” he said.
“When I was doing the business I was getting profit to help my child and help my family buy food. When I got sick, it was very bad because everyone in my family was looking after me so there was no-one to help them. I didn’t have anything in that time because every time they come to hospital to bring something to me, they used the transport.
“Sometimes in my house there was no food and no one to look after my child it was a very bad situation. Something like this affected me, which is why I never go far. The one I was doing business with is going very far now and he has a big business. I am still here at home with the lockdown and not doing any work.”
He had never heard of listeriosis before getting sick.
“The time it was starting I saw it on TV but I didn’t know anyone who got listeriosis. I heard about it and some of the problems. In my province, I think I got it and another person. Some of the people I saw on TV were explaining about listeriosis.”
Kadango said he was not sure what the future holds for him.
“I try to go somewhere and see my family and do something else. Most of the things are not the same as before I was that sick with listeriosis, it has affected me a lot. It is affecting my life because most of my friends and family said you was wonderful before. Now, you are not going anywhere and doing this and this. I say to them this thing is very dangerous,” he said.
“The family was feeling very bad and me too, I was confused too much. In my life it is only me, they all depend on me as I am the old man in the family. I also had to look after one of my brothers who was ill but he is better now. Since last time I was trying to do something like a business and if I get a job I am going to work but there are not many jobs here with the lockdown.”
(To sign up for a free subscription to Food Safety News, click here.)
]]>Nthabiseng was a person who loved family above all else. She always wanted to have kids and was blessed with a daughter, Onthathile, who turns 5 this month. Matlhogonolo Chantell and her twin sister Michell Masego Zaza are raising their sister’s daughter.
Onthathile doesn’t remember much of her mother, who at the age of 35 died from listeriosis in Oct. 2018. Her death was part of a Listeria outbreak in South Africa that was traced to Tiger Brand’s polony — processed deli meat similar to baloney.
However, it wasn’t until 2020 that the family found out what had caused their Nthabiseng’s mysterious illness. They knew only that many people in the country were getting sick.

The listeriosis outbreak began at the start of 2017 and was officially declared over in September 2018 with 1,065 confirmed cases and 218 deaths.
In 2018, Nthabiseng was a new mom trying to adjust to the loss of her mother. Her partner, Onthathile’s father, had passed away before he and Nthabiseng could be married. In the two years after his death, she would lose both of her parents.
Nthabiseng had already defied odds in having Onthathile. After a liver transplant in 2009, and constant medication in the aftermath, Nthabiseng was told she had only a small chance of being able to have a baby.
She was in and out of the hospital after her transplant, constantly having her liver checked to make sure it was still functioning properly. Her sister said the family had developed a system and routine to make sure Nthabiseng stayed healthy.
“At a certain time, she takes her meds. She exercises and drinks water. We take a walk in the park. And we pray a lot,” Matlhogonolo said.
Nthabiseng and her family lived in a suburb of Johannesburg, South Africa, where a trip to the hospital could take as long as three hours depending on the traffic. When Nthabiseng began to get sick, those hospital trips became more frequent.
Nthabiseng’s battle with listeria poisoning

“It was very quick,” Matlhogonolo said. At first the sisters tried to nurse her at home. “Trying to nurse this thing, it was out of control and they could not keep her fever down. And they were referring to her saying that her kidney and liver had become poison in the system. We thought maybe the liver was rejected by her system.”
“She would vomit a lot and she couldn’t keep food down. She lost so much weight. Her eyes were yellow. Her eyes were turning yellow, so we knew something was wrong and something was eating her,” Matlhogonolo said. “She had diarrhea, that wouldn’t stop. It was crazy. She lost so much weight because she was dehydrated.”
The sisters thought that maybe it was tuberculosis or asthma. But they quickly realized this illness was different. “She was not herself. She really changed. She also had these night sweats, like these cold sweats, and we couldn’t understand. And it just kept going on and going on.”
Nthabiseng was placed into a high care intensive care unit.
Nthabiseng’s family knew that others in the country were getting sick with something similar, but nobody could tell them what was going on. “The hospital and everything and nobody really knew what was making us sick,” Matlhogonolo said. “And we really didn’t understand.”
Nthabiseng died Oct. 16, 2018, one month after the outbreak had been declared over.
It took until 2020 for a law firm in South Africa to connect the dots and tell Matlhogonolo and her sister what happened to Nthabiseng and that it was connected to the Tiger Brands outbreak. “We found it out this last year what really happened. What really caused it.”
“They found our names in the files and that we could be compensated if we pursued them. I mean we didn’t know, because we were just trying to bury our sister and find our lives,” Matlhogonolo said. The family in a matter of years had gone from six at home to three.
“The year before both of our parents died and then our sister died, so a lot of things had happened. Our main focus was for us to like to find our feet. Try to find food. Try to make this baby go to kindergarten. My twin and I were like 24. It was too much to take in. So we just had to grow up.”
Life after Nthabiseng’s passing

Matlhogonolo wishes Tiger Brands officials had come forward as soon as the outbreak happened. She wishes the multinational company would compensate people and make the public aware that the outbreak was its fault. But she isn’t angry at Tiger Brands. “It’s not good for us to hold onto rage or anger. We understand that things do go wrong in life. But I am disappointed that a big brand like them has never stepped out and looked for people that have had their lives damaged. A lot of people lost their loved ones.”
“You can imagine as young as we were having no one to rely on, living in a society where they aren’t supporting young black women is really hard. It is a struggle.”
“Knowing that Tiger Brands have done something like this, and they have never come out and said that they are sorry. And really show remorse and compensate. I am really disappointed in their brand. I would say I am disappointed, but I am just praying that justice is going to be served.”
“What I am crying for is her child. She deserves quality education. She deserves quality life. I am being like 26 there are still a lot of things that I need to do for myself and for if I grow old. And being a student like I am, they didn’t think about how people like us really need to be taken care of.”
“They should make amends for the mistakes.”
More background information about the 2017-2018 South Africa Listeria Outbreak can be found here.
(To sign up for a free subscription to Food Safety News, click here)
]]>The three-year strategy is part of a series of steps taken by authorities, including funding a project and organizing an event, to prevent another outbreak.
Phases 1 and 2 of the control plan for Listeria Monocytogenes in Andalusia were developed by the Ministry of Health and Families.
The outbreak caused by La Mecha brand chilled roasted pork produced by Magrudis affected more than 200 people. During the alert between August and October 2019 three people died and there were five abortions.
A first phase covered the last quarter of 2019. In that period, almost 1,500 official controls were carried out with the number of food samples for Listeria doubling to more than 700 and surface samples almost tripled to nearly 400.
The aim was to raise awareness and improve the preparedness of meat companies against Listeria. Authorities said firms now have a more agile response in the event of an incident, through implementation of preventive measures and surveillance of production environments and surfaces.
Second phase
The Ministry of Health and Families developed guidelines for the control of Listeria in meat products for Andalusian companies in the sector and those involved in official controls.
The second phase, during 2020, involved characterizing all companies and their products with respect to the risk of Listeria and including this information in the official control database. Work included evaluating the effectiveness of controls adopted by the companies; verifying compliance with Listeria limits; and increasing effectiveness of official controls.
Phase 2 was extended to all those that put food at risk of Listeria contamination on the market, including the fish, dairy and vegetable sectors. The number of tests is above what was planned in 2019 with more than 1,100 Listeria samples in Andalusia for 2020. Analytical results showed 11 positives from 704 samples in 2019 and 15 positives out of 1,135 samples in 2020.
Tracking and monitoring systems have been modernized with whole genomic sequencing of Listeria strains, training and use of the FoodChain-Lab software. Work on a third phase, covering 2021 and onward, is ongoing.
Andalusian authorities previously set aside €100,000 (U.S. $113,000) for research to learn from the region’s outbreak. The project is looking at the epidemiological, microbiological and clinical aspects of the incident.
In early 2019, nearly 700 experts met in Seville to discuss Spain’s largest ever Listeria incident at the International Symposium on the Andalusian Listeriosis outbreak.
(To sign up for a free subscription to Food Safety News, click here.)
]]>James Nsayi is now 5 years old. He was diagnosed with listeriosis during the outbreak and suffers from epilepsy.
The outbreak was linked to ready-to-eat (RTE) meat products and caused at least 1,050 illnesses and 218 deaths. It was traced in March 2018 to an RTE processed meat product called polony made at a factory in Polokwane run by Enterprise Foods, then owned by Tiger Brands. In August this year, Tiger Brands agreed to sell its processed meats division, which includes Enterprise Foods.
Mario Nsayi, James’s father, said before becoming sick the youngster never had a problem with health and was a normal child.
“We had never been admitted to hospital before and never worried before. He was a good boy, playful and full of jokes. Since he became sick it has been a challenge for us as a family and then came the Coronavirus lockdown. His situation has changed our lives,” he said.
Initial illness
James is the youngest child of Mario and Emma. The oldest is 13-year-old Maxwell and 10-year-old Stalvie is in the middle.
“We normally bought polony and other sausages and James used to have it for lunch but as a young boy he used to just cut off a piece and eat it on its own so he had the plain one a lot. Sometimes Maxwell and Stalvie had it for lunch. Now we don’t eat it, since what happened I stopped buying it for the kids as I am scared something else will happen again,” said Mario, who was a tour guide in Cape Town before losing his job earlier this year because of the pandemic.
James fell ill in September 2017 and was admitted to Somerset Hospital for one month with a fever, loss of appetite, and vomiting. He then had a seizure and was sent to Red Cross War Memorial Children’s Hospital.
“He was in the intensive care unit and they discovered it was listeriosis. He was in ICU for two weeks on a machine in a coma, he couldn’t breathe himself, the machine was keeping him alive. He stayed there for two weeks and became a bit better and was sent back to Somerset Hospital. After two weeks he had another seizure. All together James spent three months in hospital,” said Mario.
“The other kids are very traumatized, it (was) Maxwell’s birthday in October. I couldn’t celebrate it because James was very sick, it was a big problem. That has affected him as well. As a child, he says my birthday is not celebrated, not even a cake for me because mum and dad are in hospital. My mother was looking after the children while my wife and I rotated at hospital. We couldn’t leave James alone as it was too serious, you are worried all the time and don’t know what might happen next.
“He lost his memory so he had to learn my name, when he came home from hospital he couldn’t remember me, his brother, he forgot everybody so it was very difficult.”
Follow on problems
About six months later, James started having seizures. He was taken to hospital before being discharged after treatment. However, after another three months, he had another more serious seizure.
“I said to the doctor we need to understand what is going on as we can’t continue like this — seizure and back. One day he’ll have a seizure and we are not there and he is gone forever. They sent us back to Red Cross Hospital and they realized his brain was affected by listeriosis and he had epilepsy.”
Nobody in the family has epilepsy, according to Mario and he wanted to be sure before giving his son treatment.
“The doctor said if you want to save your son you have to do the treatment. If we don’t do it and he has a seizure then gone, finished, he is never coming back. At the beginning we were giving him medication in the morning, lunch and evening. Six months later he had a seizure again and the doctor said the dose needed increasing,” he said.
James was started on Epilim syrup but is now taking a tablet. He will be observed for two years and treatment may be changed if there are no more seizures.
Coping and moving forward
Mario said his son is not the same since the illness.
“He is not like before. I am afraid to take him somewhere when it is too hot. I try to play soccer, rugby or tennis with him. We go in the garden to run and keep him fit. I always keep an eye on him. He is not like a normal child due to what he went through and the epilepsy caused by Listeria. For Maxwell or Stalvie I have no worries but James I always worry where is he, what is he doing, why is he quiet? The rooms are upstairs where we live and if they are watching TV downstairs every 10 minutes I must call James. It is a scared life, something else can happen if I am not there.”
At least part of the blame for the outbreak lies with the government, according to Mario.
“It is important for government inspectors to monitor food chain programs and make sure the product we are eating is safe. If the factory is not clean, it can affect citizens. At the end of the day it is extra cost for medication. Imagine, James spent three months in hospital, all that costs money,” he said.
“As consumers we go to the shops, I put what I buy in the fridge, but we cannot go and investigate. If I say I like polony let’s go and see how they make it, they’ll kick me out but the government has inspectors to make sure people like Tiger Brands are doing a proper job. The government gives them a license to make products the consumer will buy. It needs to make sure hygiene is a priority.”
Mario said it was important for other families going through similar things to find a way to cope.
“It is not something we planned ourselves, it was not our fault. It was an outbreak, there are consequences and people who fall victim of it. We need to accept it. Some people lost their lives to listeriosis and others recovered 100 percent. Unfortunately, I thought my son recovered but now he has epilepsy and this affects emotionally my life,” he said.
“As a parent we need to be courageous, James needs me and my wife and we need to make sure everything is balanced at home. We need to support the children. This Listeria story mustn’t affect James’s life or his future. I still have hope James will recover fully and one day it will be a thing of the past.”
(To sign up for a free subscription to Food Safety News, click here.)
]]>Eleven-year-old Phoebe Bettey, from Plymouth in England, went to Lanzarote with family in late July 2019. They stayed at the Holiday Village Lanzarote, run by tour operator TUI UK. One week into the holiday, Phoebe fell ill with gastric illness, which was later confirmed to be salmonellosis.
Several weeks after being diagnosed with the gastric infection, Phoebe developed a secondary condition, reactive arthritis, which is joint pain and swelling triggered by an infection in another part of the body. In most cases, it clears up within a few months but long term treatment may be needed. She now requires medication and is under the review of a pediatrician.
“Since our holiday to Lanzarote, Phoebe has struggled a lot. She is far too young to be dealing with something like this, and it is heartbreaking to know that she is in pain. Reactive arthritis was something I really didn’t know much about before last year and, like most people, I assumed it was probably a condition that older people suffer with,” said Phoebe’s mother Jane Cray.
Infected while on holiday
Phoebe was nine-years-old when the family went on holiday to Lanzarote in July 2019. At the start of August, she began to feel unwell with symptoms of nausea, a headache and high fever. She then began to have diarrhea, abdominal pain and vomiting.
Phoebe was diagnosed with Salmonella infection following admission to a hospital in Lanzarote. The family flew home on Aug. 8 while Phoebe was still suffering from loose stools and abdominal pain.
About a month after the holiday, Phoebe started complaining of puffy eyes and pain in her toes, legs and joints. She was diagnosed with reactive arthritis, believed to be linked to the Salmonella infection contracted in Lanzarote. Phoebe now takes anti-inflammatory medication and is being reviewed by a pediatrician. She continues to suffer from puffy eyes, swollen toes and painful legs and joints.
Phoebe and family have joined with their legal team at Irwin Mitchell to mark National Arthritis Week from Oct. 7 to 13 and World Arthritis Day on Oct. 12 by raising awareness of the link between the condition and gastric infections such as Salmonella, Shigella, Campylobacter, Yersinia, and Cyclospora. All can be foodborne.
“I wish I could turn back the clock and stop us from going on holiday last July, but I know this isn’t possible. I just hope that by sharing what Phoebe is going through, we will help raise awareness of the condition and the symptoms people should be looking out for,” said Cray.
Raise awareness and offer support
Phoebe’s family asked lawyers at Irwin Mitchell to investigate how she fell ill. Jennifer Hodgson, associate solicitor, said the hope was to help raise awareness of the condition and links it has to illnesses such as Salmonella.
“The past year has been an incredibly difficult one for Phoebe, firstly contracting Salmonella during a family holiday, and then to develop reactive arthritis shortly afterwards. Due to the debilitating effects of the condition, Phoebe has missed several days of school and has had to cut back on activities she enjoys, such as football, which is understandably upsetting for her,” she said.
“Reactive arthritis is often triggered by an infection of the bowel, such as food poisoning, but this is widely unknown. It is also widely unknown that illnesses such as this can affect both adults and children.”
Meanwhile, researchers recently found reactive arthritis is fueled by a protein during Salmonella infection.
Infections with Salmonella bacteria, which produce curli amyloid, are implicated in the painful inflammatory condition, which affects about 5 percent of people infected with bacteria that cause gastrointestinal illness. Very little is known about how or why it develops.
Scientists at the Lewis Katz School of Medicine at Temple University showed that in mice infected with Salmonella Typhimurium, curli provokes the generation of autoantibodies and joint inflammation. The study was published in the journal PLOS Pathogens.
The research team’s next plan is to determine if the findings translate to humans, and whether curli proteins from other pathogenic bacteria, like E. coli, are capable of generating similar autoimmune reactions.
(To sign up for a free subscription to Food Safety News, click here.)
]]>On an early summer evening in 2016, Katie Ruffolo, a 36-year old mother of three, was battling diarrhea. She had no idea this signaled the start of an E. coli poisoning that would eventually attack her kidneys and stop her heart three times. Before it was over, doctors would debate whether she faced a partial recovery or death. Her prognosis was bleak.

The next morning, Katie called her doctor and was told to go to her clinic outside Milwaukee and give a stool sample. The doctor didn’t give her any medication, worried that whatever was causing her diarrhea could be made worse with antibiotics — something doctors later attributed to saving Katie’s life.
While dealing with this mysterious illness, Katie also was watching her three children while her husband was out of town on a guys’ trip. Luckily, her husband returned by the time Katie’s diarrhea had turned bloody. On June 14, Doctors admitted Katie to West Allis Memorial hospital in Milwaukee.
Hospitalization
Because Katie had already submitted a stool sample to her doctor, the doctors in the emergency room were quickly able to figure out what was wrong. On Wednesday, June 15, results came back from the stool sample and E. coli O157 was identified.
Thursday morning, Katie was transferred to the intensive care unit because her kidneys were beginning to fail. “My keratin levels were going up and they knew I was going to need dialysis at some point,” she said.
Death’s door
On Friday, July 17, Katie was moved to interventional radiology, where they do small procedures, so she could have a port put in for dialysis. But when she lay down, her heart stopped. She coded for 15 minutes. “What they think happened is that the fluids that built up in my body were not flushing through. They told me it basically had drowned my heart and stopped it.”
The doctors were able to revive Katie, but there were other major concerns, such as brain damage from oxygen deprivation. She was placed on a ventilator for the next two and a half days. Doctors also started cooling her body and then slowly warming it up. This technique is called therapeutic hypothermia. It is used to prevent or lessen brain damage.
Heart stops again
Sunday the 19th, Katie’s blood pressure fell and she coded again, this time for only a few minutes. Miraculously, later in the day, Katie opened her eyes and responded to questions.
Thanks to her parents being able to watch her children, Katie’s husband was able to be at the hospital constantly. He only left when forced to. But then, over the weekend of July 17-19, her parents found bloody stool in Katie’s 2-year-old’s diaper. The 2-year-old and 7-year-old were tested and found to have E. coli poisoning. Fortunately, neither case was severe. “Thank God they just weren’t sick. They just needed to get tested until it was gone. So obviously we all ate something. And it obviously affected me way more than it affected them,” Katie said.
For the next few weeks, doctors worked to keep Katie alive.
“I remember one of the doctors telling me that they would start the day with 10 or 12 of them around a table talking about what they were going to do, just to keep me alive.”
Katie’s white blood cells and platelets went up and down, so she continued to get blood and platelets transfusions. Doctors had to drain her stomach fluid and were worried that they might have to remove her colon because it showed enlargement. “They put a gallbladder tube in, which I didn’t know was something they could do, which basically stayed in my body for weeks after that. Just to make sure the fluids coming from there were okay.”
On June 23rd, Katie’s colon started working again, a good sign that her colon was going to be okay. Meanwhile, however, she was on constant dialysis.
On June 28th, Katie was able to stop continuous dialysis. They started giving her dialysis as needed. Katie had fevers that would come and go, fevers they would have a hard time controlling.
“I don’t really have much memory of this time; I have little blips here and there of things. But I was also on some pretty serious drugs, rightfully so for pain and sedation. And I had some ICU psychosis happening,” Katie said.
On July 3rd, Katie started making her own urine. She became more responsive and she only needed small amounts of dialysis.
Katie’s heart stops a third time

Saturday July 9, Doctors attempted to remove her ventilator and she coded again, this time for a few minutes. “Things had started to look better, but I guess that was kind of the story, you take one step forward and then it would be two steps back. It was just constant back and forth.”Later that day, Katie was the most responsive she had been since entering the hospital. She even got agitated because she wasn’t allowed to have real food. Katie had been on IV nutrition since being put on a ventilator.On July 11th, Katie had her last dialysis. “It wasn’t quite a full month of dialysis but a good three weeks. And my creatinine numbers, the numbers they use to measure your kidney function, were slowly going down.”
Katie remained on and off the ventilator, but she still had difficulty breathing. Doctors finally decided that doing a tracheotomy might help. “They weren’t sure, and they kind of left the decision up to my husband and my parents. Basically, like we can try this and it’s not going to hurt anything. So, they went ahead and did it.”
ON July 13, they did the tracheotomy. “That was kind of like the magic key. And I needed minimal vent after that. I would go hours and days without it.” During this time, Katie started having physical therapy and occupational therapy. “After you sit in a hospital bed without moving for a month, you can’t move. They had people come in to just get me to sit, or just try and stand, or sit in a chair, or on the side of the bed.”
Coming out of the fog
On July 16, Katie started to feel more like herself. “I pulled out my feeding tube and wouldn’t let them put it back in.” They let Katie try to eat, starting with soft foods like jello and pudding.
When they took Katie completely off sedation, she still had a trachea and couldn’t talk. “I obviously had a lot of questions, but my fine motor wasn’t working the way I wanted it too. I couldn’t use my phone. To type on a phone on that touch screen is really hard. So there was a lot of frustration on my part because I couldn’t communicate what I wanted.”
On July 21, with her organs stable, Katie was transferred to another hospital in Milwaukee to start rehab. She began therapy for 3-4 hours a day while medical staff monitored her.
On July 23, Katie’s tracheotomy was removed and after two weeks, on August 6, Katie was released from the hospital.
“Once I started progressing I just started to take off. But also, I had my age working for me, being 36 at the time. I was sort of in the sweet spot. Not too young, not too old. I was a physically fit person before that and physically healthy, no other underlying health concerns, thankfully,” she said.
Home at last

At home Katie received outpatient therapy. “From talking to all the doctors and nurses, I still keep in contact with a lot of them, they said it was a once in a career case. It’s not something they are used to seeing all the time.”
They explained to Katie that in their eyes, she shouldn’t have been able to live through it. They told her it was a miracle that she didn’t have lasting physical limitations or brain damage from coding. Although, Katie explained, it did take a while for her brain to feel like it was back to functioning at the same level.
“The therapist would come and ask what day it was, and I would say, I don’t know. At one point they asked me what time it was, and I looked at the clock and couldn’t make sense of it. They would have me do things, like a puzzle or something and I remember saying, like, I can’t do this, but I know I should be able to do this,” Katie said.
But eventually it all came back. “At one point the speech therapist dismissed me, because we were working on brainteasers, and she was like, you’re fine. She was like you’re good.”
Reflecting
Katie has now had several years to reflect on the trauma she went through.
“I guess I never understood how people could die from E. coli. What is that? I think a lot of my family and friends had no idea either. So, I think a lot of people have learned a lot from what happened to me.”
Katie explained that if there was a silver lining to the incident, it was that it educated a lot of people on the importance of food safety. “People tell me they have rethought food and really think about food. I’ve had people tell me they just won’t eat romaine. Because there have been so many outbreaks in the last few years.”
Unfortunately for Katie, there’s no way to know for sure what she ate that caused her to get ill. “It is very frustrating in some ways. But not as frustrating as some people think it would be.”
“They ask, ‘What did you eat? Doesn’t it drive you crazy? Did you drive through fast-food at some point? Could it have been baggage lettuce or salad?’ Yeah, I guess. But it’s too many options to know,” she said.
“People want to hope that that can’t happen to them. But the reality is that it can happen to anyone. It doesn’t matter. And food safety is a really important thing.”
Fully recovered, Katie is back to teaching full time with no long-term health issues resulting from her fight with E. coli. Katie is now an advocate for food safety, including a close relationship with the nonprofit public health organization STOP Foodborne Illness.
STOP Foodborne Illness is the only national nonprofit public health organization whose mission is to support and engage people directly impacted by foodborne illness and mobilize them to help prevent illness and death by driving change through advocacy, collaboration and innovation.
(To sign up for a free subscription to Food Safety News, click here)
]]>Foodborne illness can really wreck a party, so we’re asking dads everywhere to brush up on their food safety knowledge. “It can happen to anyone,” says Mitzi Baum, CEO of Stop Foodborne Illness. “We are all susceptible to the dangerous foodborne pathogens that cause 3,000 people to die each year with another 128,000 hospitalized. Many continue to suffer from on-going consequences including heart disease, diabetes, gastrointestinal and stress disorders long after their illness is over.”
On our website, Stop Foodborne Illness features an honor wall, where we share the stories behind the statistics. You can read first-hand accounts of both survivors and those that succumbed to foodborne illness, including the following two stories:
Ken
Lives can be forever altered by the sudden and confusing experience of foodborne illness. Thankfully, this father lived to tell the tale. In 2011, Ken was handling raw hamburger meat, making dinner for himself and some friends. After two days of continuous vomiting and diarrhea, Ken noticed blood in his stools. At the urging of his doctor, Ken immediately went to the ER, where he was given three liters of IV fluids, and the doctors ran some tests. Two days later, the hospital had results: Salmonella. Ken was prescribed a week of antibiotics, which began his slow recovery. With help from the Maine Center for Disease Control and the 13 other cases that had arisen in nearby states, Ken determined the origin of the infection. It was a three-pound bag of ground beef, of which he had handled and cooked only one pound.
“I know we’re all here for a limited time, so I was never afraid of dying. My kids have seen me go through a lot. I keep a positive attitude to show them how to keep your balance, even through adversity. I’ve always taught them to live each day the best they can.” Ken’s children have seen him battle a monster. But, “I am still here,” he says, “and I still have the opportunity to live and put a smile on people’s faces.” Ken believes that when we come together to help one another, that’s when life is best. “My children are living happy and successful lives, and I’d like to think I had a hand in that.” Despite the trauma he experienced, he is determined to keep a balanced life and pass on a message of positivity and perseverance. Read Ken’s full story here.
Riley
Riley was 16 months old in 1993, when an E. coli outbreak dominated the news in the Pacific Northwest. Because Riley had never eaten hamburger and wouldn’t anytime soon, his dad was more concerned about his nine-year-old brother. That did not matter, however, as Riley became ill not from directly eating food contaminated with a foodborne pathogen, but because of person-to-person contamination — from another child in his daycare who was sick with E. coli. Only 23 days after he became infected with E.coli and later developed HUS – requiring dialysis, exploratory surgery removing a large part of his intestines, and being placed in a medically induced coma — Riley died from a massive brain hemorrhage and multiple organ failure. “Seeing two men carrying my young son in a white coffin on a cold February morning is an image that is forever burned into my memory. That coffin was far smaller than a coffin should ever be,” says Darin, Riley’s father.
After Riley passed, Darin refused to let his son’s death be in vain.
He became an advocate for food safety, along with parents like himself, helping the government make food safer. Over the next five years, Darin was speaking, writing, and working as a consultant to the USDA’s Pathogen Reduction Program. This experience led him, when he started teaching high school history, math and science, to bring this message with him. During his teaching years, he was certified by the FDA as a Food Science Educator and presented before legislators, industry, national organizations, and consulted with and was featured in numerous print and broadcast media. After 15 years of classroom teaching, Darin left his job and moved to the East Coast to pursue his desire to work in some capacity to prevent others from suffering from foodborne illness.
For two years, he was the senior policy coordinator for Stop Foodborne Illness. Meanwhile, he conducted and defended his doctoral research on states’ ability to implement federal food policies. Today, he is a professor of food policy, lead faculty of a regulatory affairs of a graduate program in food, and an assistant dean at Northeastern University in Boston, MA. And he is the author of two recently published books, “Food Safety: Past, Present, and Predictions” and “Building the Future of Food Safety Technology: Blockchain and Beyond.”
Darin believes that focusing one’s energy solely on the failures in the past is neither healthy nor sustainable. He says, “Supporting and inspiring those who act to prevent future failures can bring about immeasurable rewards. Our world needs these voices and their passion to help inspire the changes we all need. My drive has been to create a future where fewer families live with a chair forever empty at the dinner table.”
“I lost my son, yes. But my son did not lose his father.”
By focusing on inspiring the future generations of food safety heroes, Darin finds incredible fulfillment, but, more importantly, he also finds peace in those opportunities to still be a father to his son.
About the organization: Based in Chicago, Stop Foodborne Illness is a national nonprofit public health organization whose mission is to support and engage people directly impacted by foodborne illness and mobilize them to help prevent illness and death by driving change through advocacy, collaboration, and innovation. https://stopfoodborneillness.org/
(To sign up for a free subscription to Food Safety News, click here.)
]]>Petra Donnison, a family friend, created the Give a Little page for donations to help Grace Archer, her family and partner Theodore Warrick.
Grace is currently being treated in the intensive care unit of Auckland Hospital in New Zealand. She contracted Listeria meningitis which has led to Encephalitis while working in the Cook Islands. She is in a coma and receiving antibiotics to treat the infection, according to the donation page.
“We would like to raise money to support her ongoing recovery and rehabilitation. And also to support her immediate family as they in turn support her,” the page says. “Most of her immediate family live and work distanced from Auckland.”
The Cook Island News reported she is the country’s first Listeria infection patient in more than 10 years. The Health Ministry and Auckland Regional Public Health Service are investigating the source of illness.
Donations and best wishes flood in
Grace was medically evacuated from Rarotonga, the largest island in the southern group of the Cook Islands, where she and her partner Theo work as teachers.
Nearly 300 people have given money so far since the appeal was launched in mid-May.
“The money will initially be used to cover expenses regarding accommodation and travel to Auckland for Grace’s family. This will be re-evaluated as Grace begins her long term recovery and the ongoing financial needs for that,” according to the donation page.
Grace and Theo taught at Apii Te Uki Ou, a Ministry of Education and privately funded school on the main island of Rarotonga. “We love and miss you guys. Sending you and Miss Archer loads of love, hugs and strength,” said a post on the school’s Facebook page.
Listeriosis is an infectious disease caused by the bacterium Listeria monocytogenes. Symptoms include fever, muscle pain, septicemia (blood poisoning) and meningitis. The incubation period is usually one to two weeks but can vary between a few and 70 days.
High risk foods include pre-packed sandwiches, deli and ready-to-eat meat products such as cooked, cured and/or fermented meats and sausages, soft cheeses and cold smoked fishery products.
(To sign up for a free subscription to Food Safety News, click here.)
]]>Beulah Rhode (Roberts) started experiencing flu-like symptoms and felt constantly fatigued in mid-May 2018. She was in the hospital from June to August. In July, she went into a coma and was on life support until late August 2018. Tests while she was in the hospital were positive for listeriosis. After waking from the coma, Beulah had lost the ability to speak, read, write, and walk.
The listeriosis outbreak began at the start of 2017 and was declared over in September 2018 with 1,065 confirmed cases and 218 deaths. It was traced in March 2018 to a ready-to-eat processed meat product called polony made at a plant in Polokwane run by Enterprise Foods, which is owned by Tiger Brands.
Visits to three hospitals
Beulah, who lives in Cape Town, saw two doctors who diagnosed her with a slight fever. She took a week of sick leave but her mother, who is a theatre nurse, convinced her to go to the hospital.
“I was feeling tired all the time like I had the flu. I saw the GP before I got sick because I said why do I feel like I have the flu but I’m not really flu-ish? The first hospital said you’re fine you’ve probably got a bit of flu. At the second hospital I went into the emergency room and doctors told me the same thing. They said maybe I have the flu but I was like no it is not, something felt different,” she told Food Safety News.
 “When I went to my house, my mum called and said I want to check on you as you’re not feeling or looking well, then she took me to a different hospital and my journey with listeriosis happened.”
“When I went to my house, my mum called and said I want to check on you as you’re not feeling or looking well, then she took me to a different hospital and my journey with listeriosis happened.”
The 35-year-old was in hospital for three months and physical rehab for two months to learn to walk, talk, read, write and how to use a knife and fork again. She was discharged in October 2018.
“That was very frustrating as I have always been motivated and able to do everything for myself. In my life before I could take my three dogs and go and walk with them. I don’t have the physical ability to do this the way I used to before. After rehab I was at home for five or six months and then the company I was working for gave me temporary disability for that period I was not working,” said Beulah.
“During that time I was thinking would I be able to do my job again because the listeriosis affected my brain. I realized it was so difficult because I couldn’t send a text message from my phone because of the spelling of a word. I have a bachelor’s degree in law, I was enrolled to do my Master’s degree and suddenly I couldn’t spell a simple word.”
Going back to work
Beulah said her job as a qualified advocate involves a lot of responsibility and there was no replacement cover in the time she had off. She returned to work in February 2019.
“I was under pressure to pick up where I left off but with the brain having an injury it is impossible to do that. That is the hardest part, my brain wasn’t performing the way I was used to and the same thing for my body,” she said.
“I’ve been blessed in many ways but my biggest challenge is the brain doesn’t recover as quickly as, especially employers, think. Because it is not a physical injury they can see like a broken leg, if it’s a brain, emotions or self-confidence they can’t see that but you feel it.
“For me, every day when I walk into my floor and office it is “oh, here we go” it takes a lot of courage to stand up in a room and speak about things I am struggling to remember. The good thing is it has cleared up a lot of things in terms of what we are lacking, especially in labour law and I could focus on that for a Master’s degree topic when I am ready to commit to it.”
Beulah said the first six months back at work were “terrible” as she was a shadow of her previous self.
“It was very challenging and traumatic because I didn’t know what was happening, I didn’t understand myself because part of your brain is still not processing what’s happened because half of it you don’t know due to the coma. When I did come to I was on life support, so a lot started opening up in terms of what actually happened in that time and that obviously affected me emotionally.”
Beulah’s neurologist and physician recommended she see an expert for a neurocognitive assessment.
“I went to see him in August last year and we did a three hour session with exercises on how the brain responds to questions, lighting, memory and all those things. He provided a report on my capabilities at that stage which were very poor compared to before the incident,” she said.
“He recommended a follow up within six months. The six months after August were very traumatic. I had an epilepsy episode at work in late August as a result of listeriosis which left a scar on the brain and that is causing the connections from the brain to the body to sometimes go crazy.
“Three weeks ago I was in hospital for a week with migraines, my neurologist did another scan and he said it was the scarring that was causing it. A week ago I went to the neuropsychologist for my follow-up assessment and he gave me a very good report. There are a lot of functions that are not at 100 percent yet but I have increased by 80 percent compared to the exercises we did in August.”
From death’s door to marriage
Beulah got married to Envor Rhode this month. Speaking before the big day, she described the occasion as bittersweet.
“It is quite bittersweet because I am thinking this is the most special day ever. But will I have a headache now the whole weekend? If I think about my quality of life, we have expectations, we want to have kids and we want other things and not just a career but what is the quality of that life when you have to lie down if you have a headache, when you have to be careful as your head can’t get hurt again. It’s things that you’ve never considered and you cannot put a value on it,” she said.
“I have good medical aid so got the best care I could get and not everyone has that available. The same with support at work, a lot of people don’t have the support that I had. I had an income for the entire time, businesses close all the time and if you are sick for nine months they are just going to get rid of you but I walked right back into my job.”
While she was in the hospital Beulah’s parents were called by doctors to say farewell to their daughter. However, hopeful she would regain consciousness they kept her on life support.
“I was resuscitated twice in hospital, putting my parents into a tail spin, as Beulah doesn’t get sick but she is in ICU. It is very traumatic, my mum hasn’t got over it. I was at death’s door and now I am getting married. It affects your complete life, your perspective and you either go off on a tangent or you can rise up and I’ve made the decision to rise up. Unfortunately, the listeriosis did not end, it continues every day. My follow-up got cleared, it is out of my body and system but the side effects are still there.”
Emotional journey
Beulah said the third hospital trusted what she said about not feeling well and knowing something was wrong and despite not knowing what the problem was they were determined to find out.
“They did so many tests. My mum was sitting by my side morning and night. My family supported me so much, especially my mum and dad they just believed this is not it for Beulah, she has worked too hard,” she said.
“To myself there were a lot of questions, I was at the top of my game when I got sick so I was confused, why did this happen to me? In hospital and rehab there are a lot of nights lying awake, everyone is sleeping around you, and you are trying to figure out what am I doing here? Look at all these people that can’t walk or talk properly and then I thought oh but Beulah that is who you are right now. In a sense you feel angry, what did I do to have that happen to me and yet it did.”
Initial details about the outbreak were not clear, according to Beulah.

“There was news about it but there was never a name for it, they were saying there is a virus and people must be careful what they are eating but you never heard of someone it happened to, so it didn’t seem like it was here. Even when people heard it happened to me, they couldn’t believe it and didn’t know what it actually was. So we didn’t know enough about it, where we would be at risk and that it was as deadly as it is, it was the last thing on anybody’s mind,” she said.
“I ate polony and a lot of other meats. They wanted to know exactly what I ate and I said I was a single woman living on my own, I would go to the shop and buy things for the month. So when I come home late at night I would throw something in the microwave. It could be a pasta meal or a sandwich. No I don’t eat it now, absolutely not and I don’t buy any brand of polony.”
Beulah said her perspective on life has changed in many different ways and she is looking forward to married life.
“You realize you don’t have as much time as you think and you are here today so make it good. You can have all the cars, titles, degrees and jobs but if you don’t have your health it doesn’t matter what you earn or own or who or what you know,” she said.
“For me it was accepting you are where you are now, so what do you want to do for the next 35 years and I don’t want to spend them running around from 5:30 in the morning and leaving work at 7 or 8 o’clock at night and coming home to feed my dogs, talk to them for a few minutes, have a bath and go to sleep.
“We don’t have kids, we are hoping that is going to come. That is one of the things I shifted aside because of my career. It has to wait until the doctors give me the go ahead when my body has fully recovered. We are working on my health to get it to the optimum level and once the doctor says I am ready then we can try.”
(To sign up for a free subscription to Food Safety News, click here.)
]]>Petra Bischoff was admitted to the hospital in May 2017 and diagnosed with Listeria meningitis.
She was in the ICU for nearly a month with 20 days on ventilator support. Petra went into a coma and was paralyzed when she woke up. The paralysis extends to Petra’s vocal cords, which makes it difficult for her to speak for any length of time.
‘To be a baby at 69 isn’t easy’
Petra, 71, said listeriosis has ruined her life and that of her daughter.

“I was a very active and happy woman and I cared about my appearance and my health. I ate healthily and exercised regularly. I liked to appear well-groomed and dressed. All of that changed,” she told Food Safety News.
“I was ill two months beforehand and we didn’t know what was wrong. I was feverish, with muscle pains and headaches, an upset tummy and I ended up in hospital. To be a baby at 69 isn’t easy. When I look in the mirror I look at a strange person. I don’t know this person.”
The listeriosis outbreak began at the start of 2017 and was declared over in September 2018 with 1,065 confirmed cases and 218 deaths. It was traced in March 2018 to a ready-to-eat processed meat product called polony made at a plant in Polokwane run by Enterprise Foods, which is owned by Tiger Brands.
Corne, Petra’s only child, said she noticed something was wrong as her mum was very run down and not like she used to be. The pair live together in Cape Town.
“All of a sudden she started being very tired and lethargic and didn’t want to do anything, just lie down. My mum has more energy than me and she is 30 years older but that did change a month or two before May you could see she was starting to become just despondent with everything and we couldn’t figure out what was wrong.”
Re-learning to walk and talk
Petra was in hospital and rehabilitation for three months including the time on ICU mostly in a coma, one month on a hospital ward and a month in another hospital for rehab.
“In the hospital they rehabilitated her and taught her how to speak, walk and eat again. I visited her every day, I was there more than I was anywhere else. She had to learn everything new because the doctor had explained if your body lies still for so long all the muscle mass goes, so they had to build the muscle mass and retrain the body to do everything. She was very frustrated, angry and stressed. It was very taxing on her, it still is,” said Corne.

“She can’t hear or speak very well due to the damaged vocal cords, her eyesight is very bad so she doesn’t have that quality of life. She doesn’t have good mobility and walks very slowly, her hands sometimes cramp up and we have a full time carer here every day. She’s far better than what she was but it’s still not so that I can leave her alone as sometimes she gets dizzy and bumps into things and she bruises and bleeds easily.”
Petra trained as a color and line consultant in the fashion industry. After working in the real estate industry for 25 years she planned to direct her attention toward her love of interior design and start a business. Petra had bought specialized software to present 3D renderings of designs to clients, and done a course in home staging and property styling.
These plans have been abandoned and Corne lost her job after taking time off to support her mother. She now works in skills development but also used to be in property.
Lifestyle impact
Corne said she has been left mostly alone to deal with her mum’s illness and the heavy financial burden has involved selling property.
“Because she is now a full time responsibility I don’t really go out a lot any more, I was very sociable but now I prefer to stay here to keep an eye on her. I’ve lost quite a few friends as nobody wants to visit someone who is not 100 percent well and fun. This has isolated us in some ways because a lot of her friends don’t know how to cope as she can’t do all the activities she used to with them.
“My mum had a lot of friends and now she has one friend left who is in the medical profession, she is a retired nurse, but the others are few and far in-between to come visit. It is because she gets tired very quickly, her voice goes, she can’t hear them well or walk for long periods of time, so she can’t go out as often and everywhere she used to.”
Corne had not heard of Listeria before being told of the diagnosis by a specialized physician but the pair ate cold cut meats regularly.
“Back then I would buy once a week what we called a mixed packet of the olive loaf and I would take some with the polony and some with the peppers in and curry brawn so there was a variety that she could put on her sandwiches in the day if she was at home. Every week we would buy cold cuts. We will not buy or eat any processed meats now, if we want something like ham I will buy gammon, cook it and cut it up.”
Bearing responsibility: ‘I didn’t get my mum back’

Tiger Brands should bear responsibility after they put the public in danger, according to Corne.
“Apart from the fact so many people have died it is also the quality of life for those who contracted listeriosis is so bad. If I look at my mum, I didn’t get my mum back. So they should take responsibility for this and the Listeria in their plant. They should have pulled those products so people wouldn’t buy it,” she said.
“Tiger Brands bears the biggest responsibility but our government and the health department should also be brought to book for this as well because they obviously didn’t do all the tests that needed to be done to check the health and safety of those plants.”
Corne said the future at the moment is looking pretty dire.
“Her medical costs between the carer and the medication, vitamins and minerals to keep her going are high, as it compromised her immune system. It has affected everything. So financially it has ruined us. I couldn’t finish my degree because I have so many costs to cover that I can’t still pay for my studies so my career path ended as well,” she said.
“It is also a big emotional burden because I don’t ever know in the morning when I go if I am going to be phoned if she is not alright, does she need to go to hospital, she is ill a lot and depressed a lot which makes me depressed a lot, so it has diminished our quality of life and made us withdraw socially.”
(To sign up for a free subscription to Food Safety News, click here.)
]]>Cheryl Tavakoli paid tribute to her husband ahead of a pre-inquest review hearing.
Niptoon Tavakoli, of Lindholme, Doncaster in England, died in a hospital two months after falling ill complaining of sickness and diarrhoea.
The 65-year-old had eaten duck eggs bought from a stall at the Messingham Show in North Lincolnshire five days before becoming ill.
‘Massive hole in our lives’
Cheryl, 60, said seeing Niptoon so poorly in the last few weeks of his life and being powerless to help was truly horrific.
“Niptoon was the most wonderful, loving and caring husband and stepdad we could have wished for. He was never happier when spending time with his family or visiting antique centres and fairs,” she said.
“Niptoon has left a massive hole in all our lives and we miss him so much. We had so many plans for the future still, but now he is no longer with us, these will only ever remain as plans. It is difficult not to think that he was taken too soon.”
Niptoon, who had worked in the catering industry and retail management, bought six ducks eggs at Messingham Show in June 2019 and cooked and ate four of them.
Five days later an ambulance was called to his home but Niptoon did not go to hospital. On June 10 he was taken to Doncaster Royal Infirmary after paramedics were called again. Doctors found evidence of Salmonella. Niptoon was admitted to intensive care. However, his condition deteriorated and he died of organ failure on Aug. 12.
Provide the family with answers
Public Health England investigated and confirmed a second case of Salmonella in the West Midlands with the same strain but was unable to trace the source of the pathogen.
Cheryl said knowing another person contracted Salmonella after eating duck eggs adds to the concerns about Niptoon’s death.
“We know that nothing can ever make up for what has happened but we need to know if more could have been done to prevent his death. We know that the inquest process is going to be an emotional time but it is something we have to do to honour Niptoon’s memory,” she said.
Cheryl has instructed lawyers at Irwin Mitchell to investigate and support the family through the inquest process.
Tim Annett, from Irwin Mitchell, said Salmonella can cause serious health problems and in the worst cases, can lead to death.
“Understandably Niptoon’s family has a number of concerns about the events that unfolded in the lead up to his death. We are determined to provide the family with the vital answers it deserves and the start of the inquest process is a major milestone in being able to do this,” he said.
“We will continue to support the family throughout the process. If during the course of our investigations any issues are identified it is vital that lessons are learned.”
(To sign up for a free subscription to Food Safety News, click here.)
]]>Elizabeth Matthee, 73, fell ill in January 2018 and was in and out of hospital until early August of that year. Doctors initially thought the source of illness was her knee, but in March 2018, she was asked to return to hospital because tests confirmed she had listeriosis.
Elizabeth lives in an old age care home. Prior to her illness she enjoyed reading and watching TV and used to sit outside chatting and laughing with others at the home. The pensioner was able to move around with assistance. Her immune system has been severely hampered by listeriosis and she now depends on full-time care.
The listeriosis outbreak began at the start of 2017 and ended in September 2018 with 1,065 confirmed cases and 218 deaths. It was traced in March 2018 to a ready-to-eat processed meat product called polony made at a plant in Polokwane run by Enterprise Foods, which is owned by Tiger Brands.
Emotional impact
One of Elizabeth’s daughters, Christina Tiana Verhave, said she was a very bubbly, cheery type of person.
“We had absolute hell with touch and go situations continuously. This took a toll on my mother’s will to live, her spontaneity and her outlook on life in general. You could hear her laugh when you walk down the hall and everybody that knows her knows she will always have a joke, doesn’t matter if she is in pain or not. This took away her spirit because she was feeling so ill for so long, and she is still not well. At one stage she told me she doesn’t want to live anymore,” she told Food Safety News.
Having some polony was part of the regular routine for Elizabeth.
“Every single night she wanted Enterprise French or garlic polony, viennas from Spar or Woolworths with bread and coffee, that was her treat and she loved to have it for supper. Needless to say she is not touching polony since she found out what happened. I can’t even dare to ask her if she wants something like that. We eat ham but I don’t like polony so what we buy for my mum is different than what we eat. I thought they cleared everything to say it is safe now but I will never ever buy it again,” said Christina.
In and out of hospital
Elizabeth was first admitted to hospital in February 2018 due to an infection in her knee. The same month she was hospitalized with a urinary tract infection and more knee problems.
In early March, blood tests showed she was positive for Listeria monocytogenes and after three weeks of treatment she was discharged. At the end of the month she was admitted again complaining of constant severe headaches, vomiting, and diarrhea. Her blood culture was negative for Listeria but a stool culture showed Clostridium difficile toxin. She was discharged one week into April.
Elizabeth had to go to hospital several times in April and May complaining of leg pain. She was readmitted in mid-June with complaints of nausea as well as stomach and leg pain but insisted on being discharged.
She was admitted again one week into July for symptoms of pneumonia and herpetic pharyngitis. She had developed sores in her mouth and had not been eating properly. Elizabeth remained in hospital until early August.
Christina said she was in and out of hospital with her mum and it was a never ending story.
“It was a long, long trial for us to get her to be healthy again. Now the knee is acting up again, it is smelling so bad, and I have another appointment at the hospital for a check-up,” she said.
“At first she fell ill with fever, we didn’t know what was going on so we took her to hospital, they couldn’t find what was at fault but they gave her some antibiotics and sent her home. We went again and eventually the second or third time as they were loading her into the ambulance, her knee where she had a previous knee replacement, the scar popped open and started draining. When they took her in hospital they did a swab and tested it. They sent her home again and it took a couple of weeks before they realized that she had listeriosis. The doctor phoned me and said I must bring her back immediately.”
Elizabeth’s treatment was further complicated by the fact she is allergic to penicillin, one of the antibiotics used to treat listeriosis.
“In hospital she was lethargic, she did know who I was but she had stories in her head that weren’t true and she got aggressive at a stage. They said it was the listeriosis treatment she was on,” said Christina.
“There was a fluid build-up in her ear drums because of the infection. So she couldn’t hear when we were talking to her and that made her more anxious and upset. We had to put our mouth by her ear and talk really loud for her to hear a kind of noise. She didn’t know what was going on around her.
“I’m with my mum every day at hospital, I sometimes drive there twice a day because the health care here is not good. I go and check up on her and see she is eating and drinking and I feed her if I need to and brush her teeth. I just look after her, I can’t not do that, I will never sleep if I were to leave her and not see her every day and know she is alright. I can see my mum is going downhill. I can feel when I touch her arms that her bones are brittle.”
A lasting memory
Christina said there is one occasion that she particularly remembers.

“One night I remember, it was a Thursday, the old age home phoned me and said you must come to your mum, so when I got there she was out of it completely and it looked like a dead person lying in the bed. I saw her a week before, I used to fetch her to us at least every second weekend as we are a very close family and she was always game if you say lets do this or that,” she said.
“We phoned the ambulance service and they didn’t come. I was actually praying the Lord would take my mum because it was difficult for me to look at her and see she can’t really breathe.
“The next morning we were sitting by her bed waiting for the ambulance to come. It came Friday evening and then I sat next to her bed at hospital and in the ER until 11 that Saturday morning and a doctor still hadn’t come to see my mum. I had to go home and when I came back nobody knew where my mum was. They put her in a room that was almost like a storage room and left her there. When they read on her chart she had listeriosis they secluded her from everybody else and forgot she was there. She didn’t have her medication that she should have every four to five hours. It was horrifying to find my mother in that condition. We had so many bad experiences in hospital.”
Christina said she had heard of Listeria on the news but didn’t give it much attention.
“It was only when the doctor said your mum has listeriosis I said will you refresh my mind and then it all dawned on me. Since then people have been treating her differently because they are scared to be close to people with Listeria, they think she is contagious. It was an experience, we had to explain to staff working with her and people sharing the room that they are safe and she can’t infect them.”
Christina is a single mother, working long hours in a bookkeeping and accounting job and she sometimes relies on her sister to help with her 11-year-old son.
“You have to be strong and carry on for your family’s sake. It gets to a point where I work in the evening and at weekends and rush from the hospital to work and back to hospital and then I come home and see everything is sorted with my son. Tomorrow morning you get up at 5am and start your day, I go to the hospital before work to see she is fine and then to work, sometimes I will go during lunch if I know I can’t make it after work. I don’t know what the future holds, I am just trying to survive from one day to the other.”
(To sign up for a free subscription to Food Safety News, click here.)
]]>
When doctors told his wife Belva that Munro had died because of massive intravascular hemolysis and a liver abscess caused by a Clostridium perfringens infection, she couldn’t understand how it had happened. She couldn’t understand how he had gotten infected by Clostridium perfringens. Doctors explained that because of his diabetes Munro was the perfect host for the bacteria. They said the infection was from something he ate and they explained that the bacteria multiplied so quickly Munro did not have a chance.
“I think people who are diabetic or have an autoimmune disease or survived cancer should be able to eat in downtown Charlotte without fear of dying,” she told the doctors.
How Belva and Munro met

Belva met Munro 30 years ago at a church Christmas party. Munro introduced himself and told Belva that he thought he knew her. “I found out he’d only been in Charlotte no time, so I thought, oh, he’s shooting me a lie, here, at a church Christmas party.”
Despite Belva’s reservations, the two exchanged names and numbers. Munro would end up dating someone else until March, but after that relationship ended Belva and Munro began talking on the phone.
“He would call me every night. And talk for 30 or 40 minutes. But he never asked me out.”
Finally, Munro did ask her out. He asked her to join him at a Fourth of July picnic party. Belva described Munro on the date, “He was shy and a hunk. An absolute hunk.”
The two won a Fourth of July costume contest at the picnic.
From there Belva recalls things moving quickly. She said she knew by September that if things kept progressing, they would get married.
“He wanted to marry me and I told him that if he wanted to marry me now, he’d want to marry me in a few months and we could wait. And I told him, not to pray that we got married, pray for God’s will. And I didn’t trust him. So I told God, I said, if he’s over there praying for us to get married, don’t listen to him.”
Belva wanted a sign that she was supposed to marry Munro. Whether it was finding the perfect wedding dress by accident or being able to book the best wedding photographer in Charlotte, Belva got multiple signs. “There were so many things, it was uncanny. I just knew that it was what I was supposed to do.” Munro and Belva were married Oct. 6, 1990.
Family life

When marrying Belva, Munro became a stepdad to her two teenage daughters.
“They loved Munro as their own father. He loved them like they were his.”
Belva says that Munro was the role model her daughters needed. “They got to see what a good man was like.” “He was a great father. He was very loving to them and if they called, he would want me to put them on speakerphone so he could hear every word.”
Munro always supported Belva’s passions including her love for oil painting. He urged her to pursue art. Belva explained that their relationship wasn’t always perfect.
“Don’t get me wrong, there were times when he would have paid someone to take me and vice versa, but it was a wonderful marriage. He always seemed to love me more. And all my girlfriends loved him because he was cute as a button. And was obviously in love with me, and that’s attractive to a woman, to see a man in love with his wife the way he was with me. He adored me. He loved me with all of his heart, and I loved him the same.”
Munro’s death
On Monday, March 9, 2015, at the age of 50, Munro went to Subway with a friend where he ordered and ate a meatball sandwich. He began feeling ill that night. Munro and Belva attended a midweek church service and friends told Munro that he wasn’t looking well. The next two days Munro felt ill — abdominal cramps, nausea and vomiting. Belva was gone all day Wednesday. When she returned home, she found Munro laying on the bed. He called his doctor to ask what kind of medication to get from the pharmacy because he felt so ill.
Belva offered to accompany him to the store but he told her to stay and socialize with his sister and her husband. “The thing that kills me is I didn’t even hug and kiss him.”
Munro threw up at the pharmacy and came home in even worse condition.
“We were going to eat and he didn’t feel like eating, so we were eating and he’s lying on the couch and feeling worse.” Belva told him that he would be able to attend his Bible study in the morning. He told her that he knew he would and began to yell out in pain.
Belva took Munro to the emergency room. But as they exited the car, Munro laid on the parking lot ground. Belva ran and found a police officer. The office instructed medical attendants to get a gurney and followed Belva out to Munro.
They rushed Munro into the emergency room and started tests. Belva remembers hearing them say, “That can’t be right,” as they rushed about. He was quickly transferred to the intensive care unit. Belva recalls a team of at least 17 devoted to her husband that night — surgeons, internists and nurses.
“I had no idea what was going on, and I told him to hang on. I told him to fight. And then a flash was maybe this is it? And I just pushed that right out of my mind. Because that’s ridiculous. I begged him to hang in there.”
Belva called Munro’s doctor and good friend and told him, “Munro is in the ER and he’s very sick.” He told Belva that he was trying to have some time off, but he listened to Belva and told her, it’s probably gallbladder. Belva said she would tell Munro. “I went in there and I said, Bobby just said it’s probably your gallbladder.” But he didn’t get better and early in the morning he had to be revived.
“I talked to him about holding hands. We would hold hands and watch TV and movies and eat popcorn. And I was begging him to stay, for that.” At 9 in the morning, Munro passed again, and this time was not revived, just 12 hours after entering the hospital.
Munro’s primary doctor and friend called crying. “He had gotten up and checked things, about an hour before Munro died. So he knew when he called that Munro probably wouldn’t live.”
When a stunned Belva asked the doctors what had happened, she was told they needed to perform an autopsy.
Clostridium Perfringens — How doctors traced it back to the meat sub

The causes of death were noted to be the liver abscess caused by Clostridium perfringens infection, complicated by patchy pulmonary edema, cardiomegaly, bilateral pleural effusions, and diffuse cutaneous erythema.
The incubation period for Clostridium perfringens infections is 6 to 24 hours.
Such manifestations of C. perfringens infection are rare but well-documented in the medical literature. Munro’s C. perfringens infection was most likely the result of the consumption of the Subway meatball sub sandwich.
C. perfringens is the third most common cause of foodborne disease in the United States. It is estimated to cause almost 1 million illnesses per year. Munro’s illness began with gastrointestinal symptoms, which makes a food item the most likely source of the C. perfringens.
The time it takes C. perfringens from ingested until the first illness symptoms begin C. perfringens ranges from 6 to 24 hours. The time from when Munro consumed the meatball sub sandwich to when he first became ill fit within that time frame.
The types of food that most commonly serve as sources for C. perfringens infections for people are meat and poultry, and food items that are made from or incorporate meat and poultry.
“They told me what the germ was. Then they told me that it has a biological, it has a timestamp. And it doubles every seven minutes. So that’s exponential growth.”
Belva was told Munro, as a type 1 diabetic never stood a chance.
“They said that he was the perfect host because he is diabetic. And they said people that are diabetic, or have an autoimmune disease, or have survived cancer are perfect hosts. And I said I think people who are diabetic or have an autoimmune disease or survive cancer should be able to eat in downtown charlotte without fear of dying.”
Aftermath

“I pretended that he wasn’t dead. That he was at home or at work. I could not accept the fact. It was too devastating. I couldn’t take in the fact that he was really gone. It took me a long time before I could say or really admit that he was gone.”
Munro’s funeral was attended by the greatest number of people in the church’s history — a building that seats 720, had standing room only. Belva recounted a conversation with her and Munro’s young grandson at the service.
“I said to my little grandson, ‘Your grandfather was very, very handsome. Do you think all these people came because he was handsome?’
“And he said, ‘No.’
“I said, ‘Like your grandfather, you’re very handsome. Like your grandfather, you’re very intelligent. Do you think they came here because he was intelligent?’
“He said, ‘No.’
“I said, ‘Like your grandfather, you have a wonderful heart. So do you think they came because of his heart?’
“And he said, ‘Yes.’
“And I said, ‘Yes, so go out and make a mark with your heart.’”
Munro will be remembered forever by his wife, daughters and grandkids, as well as those in the Charlotte community.
“I’ll love him forever,” Belva said. “He was a wonderful man. People saw the love he gave me.”
After his death, art helped Belva get through difficult times. Belva’s work can be seen here.
(To sign up for a free subscription to Food Safety News, click here)
]]>If you haven’t heard, a Seattle attorney is petitioning the USDA to make it illegal to sell meat and poultry that is contaminated with Salmonella.
Yep, as of right now — and who knows how much longer — it is perfectly legal to sell you hamburger, whole hogs, turkey legs, chicken strips, and any other meat or poultry product if it is contaminated with this infectious bacteria. Even if they know a product is contaminated with Salmonella, producers from single-family farms to the world’s largest meat manufacturers are allowed to sell it.
Today I will share some of the petition, a legal document, focusing on the human suffering it represents through the stories of five victims. You can read the full petition and all of the 62-pages of legalese, but if you want to zero in on what Salmonella infections do to people, keep reading through a bit of background here and you will find the faces behind the petition.
To borrow an expression from the previous century:
If you’re not outraged, you’re not paying attention.
The bottom line is that the government hasn’t declared Salmonella to be an “adulterant” in meat and poultry, so it’s considered an OK ingredient. Tongue in cheek use of ingredient there, in case you missed the implied emoticon.
Full disclosure here, the Seattle attorney who is handling the USDA petition for three consumer groups and five victims of Salmonella poisoning is the publisher of Food Safety News. His name is Bill Marler and you can read about him in this profile the Washington Post published yesterday under the headline “He helped make burgers safer. Now he’s fighting food poisoning again.”
The plaintiffs on the petition are victims Rick Schiller, Steven Romes, and the Porter Family. The consumer advocacy groups petitioning for the change are Food & Water Watch, the Consumer Federation of America, and Consumer Reports. Specifically, the petition asks the USDA’s Food Safety and Inspection Service to declare the following outbreak serotypes of Salmonella as adulterants in meat and poultry products:
Salmonella Agona, Anatum, Berta, Blockely, Braenderup, Derby, Dublin, Enteritidis, Hadar, Heidelberg, I 4,[5],12: I :-, Infantis, Javiana, Litchfield, Mbandaka, Mississippi, Montevideo, Muenchen, Newport, Oranienburg, Panama, Poona, Reading, Saintpaul, Sandiego, Schwarzengrund, Senftenberg, Stanley, Thompson, Typhi, and Typhimurium
The faces behind the petition
Rick Schiller, Salmonella Heidelberg, 2013
Rick Schiller was one of the hundreds of people sickened in March 2013 in a Salmonella Heidelberg outbreak linked to poultry distributed by Foster Farms. The outbreak spanned more than a year and sickened 634 people in 29 states and Puerto Rico. At least 240 victims were hospitalized, according to the Centers for Disease Control and Prevention.
On Sept. 27, 2013, Rick was diagnosed with gastroenteritis, yet did not seek medical treatment as he was convinced that he was suffering from a mild case of food poisoning. Rick could not have been more wrong.
On Saturday night, Sept. 28, 2013, Rick went to bed early, hoping to feel better in the morning. When he woke up the next day, his right knee was painful, reddened, and warm to the touch.
On Sunday night, Rick went to bed with his right leg propped up and an ice pack on his knee. In the middle of the night, he was awakened by a sharp pain. When he pulled back the covers, he was startled by the sight of his own body— his right leg was dark purple and swollen to about three times its normal size. Rick’s fiancé immediately dialed for an ambulance, but Rick thought it would be faster to have her drive him to the emergency room. However, this was no easy feat. Rick recalls the agonizing experience:
“I couldn’t get my leg into the car because it wouldn’t bend. I leaned over into the driver seat and (my fiancé) had to force my leg into the car. It was excruciating. At the hospital, it took five people to help get me out of the car and into the ER. As soon as I got in there, they pumped me full of morphine for the pain, then they put Novocaine in my leg and attempted to tap the knee.
The first needle they stuck in didn’t work, so they got out a bigger one. They pulled on the syringe and meat- like stuff came out. It was excruciating, even on the morphine.”
Rick was in so much pain that he felt like he might die. After being admitted to the hospital, Rick took out his cell phone, snapped a photograph of himself, and proceeded to draft a Last Will and Testament on his phone.
During his time at the Kaiser San Jose Medical Center, Rick developed a very high fever. He recalls an unpleasant memory of being covered head-to-toe with ice packs. He continued to have pain all over the right side of his body. Both his right leg and right arm were painful. His right eye would crust up and his right ear had intermittently muffled sound.
The following day, doctors ran blood work and performed an arthrocentesis, a duplex Doppler sonography, and an MRCP (magnetic resonance cholangiopancreatography) on Rick.
On Oct. 2, he was diagnosed with colitis — localized Salmonella infection — and arthritis of the right knee, and he was discharged from the hospital.
On Oct. 15, Rick returned to the Kaiser Medical Center for a follow-up. He was seen by Orod Khaghani, MD, who informed him that his gastroenteritis and Salmonella colitis were resolved; however, Rick was diagnosed with reactive arthritis.
A few days later, Pradipta Ghosh, MD, performed X-rays on Rick’s lower extremities and diagnosed him with bone spurring and mild joint space loss, consistent with mild osteoarthritis.
Four months after his Salmonella infection, Rick returned to Dr. Khaghani, unfortunately having relapsed with lower left quadrant abdominal pain. He also complained of decreased appetite and loose stools. Dr. Khaghani confirmed his initial diagnosis of reactive arthritis and informed Rick that he was suffering from diverticulitis of the colon. At this point, Rick’s medical bills and estimated wage loss totaled nearly $15,000.
Rick’s reactive arthritis remains symptomatic to this day. He feels as if his “entire right side is now weaker than (his]) left.” He constantly worries about his health and feels as if he never fully recovered from his systemic illness. He notices generalized fatigue and is no longer able to do the handyman work that he once enjoyed.
According to the Centers for Disease Control and Prevention, the multistate outbreak Rick was involved in lasted from March 1, 2013, to July 11, 2014. The USDA’s Food Safety and Inspection Service (FSIS) was first notified of the Salmonella outbreak as early as June 2013.
By September 2013, FSIS officials had determined that Foster Farms’ chicken was behind the outbreak, yet they were powerless and unable to force a recall of the tainted poultry until July 2014.
The FSIS did not request a recall because “despite its efforts to identify the product causing the illness, no data were available that enabled its investigators to pinpoint the types of contaminated chicken products — for example, chicken breasts, whole chickens, or ground chicken — or production dates or lots.”
In September of 2013, during a USDA-FSIS in-facility testing for Salmonella at three Foster Farms production plants in California and Washington, FSIS determined that sanitary conditions at the facilities were so poor that they posed a “serious ongoing threat to public health.”
Steven Romes, Salmonella Newport, 2018
In 2018, Steven Romes, of Gilbert, AZ, was a healthy and athletic husband, father, and insurance underwriter. On Sept. 3 of that year, he consumed medium-to-well done hamburgers as part of a Labor Day family cookout.
Two days later, Steven fell violently ill with painful diarrhea, fever, and stomach cramps. Over the next few days, Steven’s symptoms worsened. He was unable to consume any solids and was forced to lay on his bathroom floor because he did not have the strength to crawl back into bed after severe bouts of diarrhea and vomiting.
On Sept. 8, 2018, after his diarrhea progressed to bloody stools, Steven was rushed to the emergency room where urine tests revealed he was suffering from acute kidney injury. He was admitted to the hospital and his illness was determined to be one of many illnesses in a nationwide outbreak of Salmonella Newport linked by public health officials to the various ground and non-intact beef products. The manufacturer was the U.S. unit of JBS, the world’s largest meatpacker.
The outbreak spurred one of the largest-ever recalls of ground beef — more than 12 million pounds of ground beef, the meat of an estimated 13,000 animals, was recalled. The recall affected nearly 50 different JBS product lines.
There were 255 cases of Salmonella confirmed across 32 states. Twenty-nine percent of patients for whom information was available were hospitalized; 6 percent were admitted to intensive care units, and two died, according to the CDC.
Fourteen months before the recall the decades-old JBS beef plant in Tolleson, AZ, which was at the center of the outbreak, had received numerous complaints of “egregious” livestock conditions. Despite the conditions, JBS was allowed to continue producing meat for human consumption.
After a colonoscopy and three-day in-patient stay at the Dignity Health Mercy Gilbert Medical Center, Steven was finally discharged from the hospital. Unfortunately, his normal bowel habits and appetite never returned, and he was diagnosed with Irritable Bowel Syndrome. Today, Steven can only tolerate bland foods and he still occasionally suffers from stomach cramps and diarrhea.
The Porter Family, Salmonella I 4,[5],12: I -, 2015
On the afternoon of June 28, 2015, Rose and Roger Porter hosted a going away party at their home in Rainier, WA. The Porters planned on moving to Costa Rica and wanted to celebrate with their family and friends one last time.
On June 27, Rose Porter picked up a whole hog from Stewart’s Meats in McKenna, WA. The next day, Rose cooked the pig just the way she was told to by Stewart’s. Hours later, the Porters’ home was filled with friends and family, many of whom were about to become seriously ill with Salmonella poisoning. It all seemed so easy and matter of fact in retrospect, as Rose recalls:
“When (the whole roasted hog)was done, I served it up. After everyone left, I cleaned everything up and threw out any food that was leftover. We packed everything up and went to bed. The next day, I woke up with explosive diarrhea. I had a very busy day because we were packing up to move to Costa Rica. I had to get out of our house because we had renters coming in. I had to find a hotel and I was dealing with my daughter not feeling well at all. She went with me for the day because she wanted to sleep in a bed at a hotel. I had to stop every half hour to use the bathroom. Diarrhea kept up.”
Once Rose and Mikayla arrived at the hotel, all Mikayla could do was lie down. She fell asleep at 6 p.m. By 2:30 a.m. she was up and vomiting. Mikayla woke her mom up and, at 4:30 a.m. on June 30, they both headed to Providence St. Peter Hospital in Olympia, WA. Joseph Pellicer, MD, was on duty in the emergency hospital and listed Mikayla’s chief complaints as “abdominal pain, emesis, diarrhea, and fever.”
Rose explained that Mikayla had been sick since the morning before with severe diarrhea. By the evening, Rose stated that Mikayla “felt like she was on fire.” Mikayla also described having shaking chills with fever and Rose told Dr. Pellicer that she was having similar symptoms. Mikayla was miserable, wracked with body aches and pain that radiated up into both of her shoulders.
Dr. Pellicer did an exam and found Mikayla was tachycardic with a heart rate of 125 and a diffusely tender abdomen. The doctor also observed that Mikayla was dehydrated with turbid urine, ketonuria, proteinuria, and dry mucous membranes.
Despite these clinical symptoms, no cultures were sent to the lab and no stool sample was collected. Dr. Pellicer diagnosed Mikayla with “acute gastroenteritis.” Just after 8 a.m., he discharged Mikayla from the ER with a prescription for an antiemetic drug and clearance to travel to Costa Rica.
On July 2, 2015, the Porters landed in Costa Rica. Mikayla was still suffering from frequent bouts of diarrhea. Upon logging in to a social media website, Rose discovered that a party attendee’s daughter was being hospitalized for Salmonella poisoning. Rose decided to take her daughter to the local ER — Beach Side Emergency Clinic in Santa Cruz Guanacaste. Andrea Messeguer, MD, the medical director of the clinic, evaluated Mikayla and noted that she was lethargic with persistent abdominal pain in the periumbilical area. Because Mikayla was currently afebrile and able to orally hydrate, Dr. Messeguer told Rose she could watch her daughter at home.
Over the next day, Mikayla did little but drink ice water, sleep, and go to the bathroom. Unfortunately, things soon took a turn for the worse. Rose recalls:
“She started crying in the bathroom that she could not bear the stomach pains anymore and needed to go back to the doctor. She told me that she had blood coming out of her butt, that it had been that way for a while, and that she didn’t know what to do. The amount of time between her going to the bathroom went from every 20 to 30 minutes to every five to 10 minutes. She was screaming in pain in the bathroom. She said that she felt like someone was stabbing her over and over again in the stomach.”
On July 3, Rose took Mikayla back to see Dr. Messeguer at the urgent clinic and told the doctor that there was now mucus and blood in her daughter’s stools. Dr. Messeguer examined Mikayla and performed a stool smear and culture. While at the clinic, Mikayla’s diarrhea decreased in frequency and she was still holding down fluids, so the doctor diagnosed her with “bacterial gastroenteritis” until proven otherwise and sent her home.
It was not long before it was clear that Mikayla’s condition was deteriorating. By the morning of July 4, her stools were entirely bloody. Rose, once again, rushed her back to the urgent care clinic. Upon their arrival, Dr. Messeguer asked to speak to Rose privately. She informed her that Mikayla was losing a lot of blood and may need a blood transfusion. However, the clinic did not have the equipment or resources necessary to perform the procedure.
Dr. Messeguer told Rose that her daughter could die on the four to five-hour drive to Hospital CIMA San Jose, and therefore, Mikayla would need to be airlifted there.
Rose and Mikayla were both transported by helicopter to Hospital CIMA San Jose in Costa Rica. According to a memorandum written by Luis Picado, MD, Mikayla presented with a high-grade fever, bloody stools, general malaise, and moderate dehydration. He wrote: “On admission, she presented with clear signs of bacterial gastroenteritis and required intravenous rehydration and parenteral antibiotics to control the infection. Stool studies were positive for Salmonella.”
Rose does not require a formal medical record to recall how things went for her daughter over the next several days. The memory is still fresh in her mind:
“For the next three days, I sat back and watched as my daughter cried in pain. I changed her bloody sheets when she couldn’t make it to the bathroom. I didn’t sleep for the first couple of nights because I was so scared that she wouldn’t wake up. (She) couldn’t process food or water. The doctor told me that the bacteria had gotten into her system and shut it down completely. When she ate or drank, it would go straight through her. She wasn’t getting any nutrition or hydration.
“The good news is that she is out of the hospital now. We have cut all pork out of our diets and are fearful of chicken and eggs. I have dealt with a husband over in Afghanistan and this was still the scariest thing I have ever been through.
I can’t say that I know what it is like to have a child die, but I do know what it is like to see a child on their deathbed.
“I have spent the last couple of months going over every detail that has happened over those two weeks. I felt totally responsible when this happened. I had to question all of my decisions as a mother. I felt like I poisoned my own child and everyone else that ate at my house. I lost friends from all of this. It was weeks later that I found out that, in the end, it wasn’t my fault.”
During the time of Mikayla’s illness, Rose and Roger had their own Salmonella illnesses to contend with. On the helicopter ride to the hospital in San Jose, Rose’s blood pressure plummeted, and she lost consciousness. Roger had gastroenteritis with uncontrollable diarrhea for several days. Rose and Roger still suffer from periodic bouts of severe diarrhea.
The Porters were three of 152 diagnosed victims of a nationwide outbreak of multidrug-resistant Salmonella I 4,[5],12:i:-. Stewart Meats’ distributor of whole hogs was Kapowsin Meats.
Laboratory testing of environmental samples at Kapowsin Meats by the Washington State Department of Health confirmed the presence of Salmonella I 4,[5],12:i:- in the facility. As a result of the investigation, Kapowsin Meats voluntarily recalled more than half a million pounds of pork products.
No wonder the petition requests an expedited hearing, calling the situation with Salmonella contamination “an imminent threat to public health necessitating prompt agency action.”
(To sign up for a free subscription to Food Safety News, click here.)
]]>“In the Marine Corps, I’m seen as the other. Being a recruit is derogatory until you finish training, you’re worthless. They break you down to build you up but it’s not fair if you don’t get built back up,” Browning said recently.

In Oct. 2017 an outbreak of E.coli O157:H7 swept through the Marine Corps Recruit Depot in San Diego and Camp Pendleton. According to the Centers for Disease Control and Prevention, there were 62 confirmed cases, 62 probable and120 suspected cases. Thirty people were hospitalized and 15 were diagnosed with HUS, a type of kidney failure known as hemolytic uremic syndrome. Patients’ ages ranged from 17 to 28 years with a median of 18 years. Consumption of undercooked beef was linked to the outbreak and was traced back to a single ground beef supplier at the Marine Corps Recruit Depot in San Diego.
One of the victims of this outbreak was Hunter Browning, an 18-year-old Marine recruit.
“What 20-year-old do you know with a full hip replacement?” Browning asked. Browning is dealing with the lifelong impact of food poisoning. “I don’t know how to deal with it. It’s not normal. When I tell people, they have a shocked look on their face and they pity me.”
In high school in Aberdeen, SD, Browning participated in drama clubs and skied in the winter. He graduated from high school in the spring of 2016. A call from a Marine recruiter convinced him that he was an ideal Marine recruit: fit, disciplined and bright. Browning was eager to challenge himself and gain the type of experience only the Marines could provide.
Boot camp
Browning took his first trip out west in the fall of 2017 to begin boot camp at the recruit depot in San Diego.
“I settled in pretty quick. I just went with the flow and tried not to screw up.” Browning said he made friends quickly, the group struggle bonding the recruits.
Marine boot camp is 13 weeks long. Browning thrived during the first phase of his training. It was not until his eighth week that he started to feel ill.
“The first symptom I showed was a fever. And then later, I was getting stomach aches,” he said.
Browning described his symptoms as increasing severe.
“They make us do this exercise at night, where they had staff that was trying to invade our barracks building. Toward the end of the exercise, I started to get this pretty heavy fever. Throughout the night, there had to be a group of four people up, making sure that nothing goes bad, or that none of the trainees leave. I was at the front post and you can’t leave when you’re doing that, and I really needed to go to the bathroom. I could feel diarrhea coming on or something. And I really needed one of the other guys to take the front post. They weren’t willing to do it because they thought I wouldn’t come back. So, it wasn’t until after I got off fire watch that I was able to go to the bathroom, and it was definitely diarrhea. Before we left the barracks I had diarrhea again, this time it had blood.”
Browning said he had never experienced pain like that. He was afraid to tell the instructor, but he was in too much pain to not. The drill inspector sent Browning to the medical center but despite running tests, they could not figure out the cause of his illness.
He explained to medical personnel that he couldn’t eat, was throwing up and had bloody diarrhea. They took his temperature and thought he had the flu. They gave him an anti-diarrheal medicine — Pepto-Bismol — a solution that Browning now realizes was counterproductive if not harmful as his body tried to expel the E. coli.
Browning stayed in bed five days before returning to physical training. Despite the pain and fever, he pushed through his physical training. But when taking off his training clothes at the end of the day, Browing noticed his legs had swollen. He recalls the other trainees’ mouths dropping when they saw how large his legs had become, from his thighs to his feet. Browing was sent to the emergency room by ambulance.
In the emergency room, blood tests were run and Browing was told that he was suffering from hemolytic uremic syndrome (HUS) connected to Shiga toxin-producing E.coli. Browning had heard of E. coli but had no idea what kind of damage it could do to his body. In just a couple of weeks, Browing says he lost more than 15 pounds, going from 165 to 149 pounds.
Contaminated food
Browning recalls in vivid detail the mess hall where he ate the burger contaminated with E.coli.
“You get your tray and your silverware, and then there’s a salad bar with a bunch of different salads or toppings for salads, and then after that, they have like a main course line, so between they’ll have like fruit sometimes, and in the morning they’ll have cereal, then the main course line where they’ll have the hot food,” Browning recalled. “And then you go past and you take a left and go past the drink machines to sit down. Then you get back up to get a drink. It’s crowded and there’s always lots of yelling. It’s very stressful.”
These details are etched in Browning’s memory because of the strong emotions surrounding that day. Browning’s life was altered because of this mess hall, the food and how it was prepared.
“There are bouts of anger, of very extreme feelings toward my situation. Because it could have been different in so many ways. If the food was cooked properly. I would be out doing my job in the Marine Corps,” he said.
The military officials held tight to the investigation process and information about it, so it was not until much later that the Centers for Disease Control and Prevention confirmed the link to the mess hall and its ground beef. Browning still remembers the hamburger and the day he ate it.
“On Saturdays, they have burger day, and that was when I got sick. I didn’t have symptoms until the Thursday after.”
Medical Rehab Platoon

After his trip to the emergency room, Browning was sent to the medical rehab platoon, where he would spend the next eight months.
Browning was in constant pain, especially in his hip joint. X-rays and MRIs revealed a divot in his femur head. He was diagnosed with septic arthritis and osteonecrosis in his hip joint caused by the Shiga toxin-producing E.coli. At first, it was the cartilage that hurt, but as the cartilage wore away, it was the femur head grinding directly against his hip that caused the pain. Standing, sitting, and any movement in between was agonizing. Browning walked with crutches or with a cane.
In late December that year, two months into his stay at the medical platoon, a hip specialist informed him that it was unlikely he’d be able to stay in the military. Browning had a hard time accepting his new reality. He recalls thinking, “I’ll get better and I’ll go back to training.”
Having not finished his training and still a Marine recruit, Browing was given little access to the world outside of the medical rehab platoon.
“You don’t have your phone. You can’t watch TV,” Browning said.
He spent his time reading and doing crafts as he waited in six-week blocks to see the doctor again. Each time the doctor told him that they would check in another six weeks.
“That was awful. You don’t know how long you’re going to be there.”
Surgery

In March 2018 – five months into his stay at the medical platoon — Browning had his first surgery. A left hip decompression was done. Calcium phosphate bone cement was injected into the femoral head cavity to provide structural support. A checkup two-weeks after the surgery showed that Browning’s hip was deteriorating quicker than initially thought. His doctor at the medical rehab platoon recommended a hip replacement. Administrative details and funding questions made Browning wait.
“There was a bit of a feud happening between the doctor and the marine corp, just because nobody in my position had ever got a hip replacement before and that’s a big-ticket item,” Browning said
Finally, in July 2018, Browning was moved from the medical rehab platoon to the Wounded Warrior Battalion where they would perform a total left hip replacement. In August, Browning had his hip replacement. His father flew out to stay with him during the surgery and help him navigate during his recovery. “It’s not like being completely fixed and mobile. That’s the struggle, knowing that it’s going to be different forever.”
Browning walked with assistance the day after his surgery. He used a walker for the first couple of weeks, progressed to a cane, and then eventually, was able to walk without assistance.
“The thing that really helped me improve was that it wasn’t painful all the time. It wasn’t bone on bone grinding anymore,” he said.
In December 2018 — after months of rehab — Browning’s doctor at the Wounded Warrior Battalion concluded that the recruit was no longer fit for service because of his hip replacement. Seventeen months after leaving home for boot camp, Browning left the Marine Corps and returned home to South Dakota where he was able to spend the holidays with his family.
Life Now

Long term, Browning will need at least one more hip replacement, and possibly two more in his lifetime. As the plastic liner inside the hip joint wears down he will endure more frequent and severe pain. Back in South Dakota, Browning can no longer enjoy the winter sports. Skiing is too dangerous for his hip. Even walking outside the house in the cold weather and potentially slipping on ice has become a terrifying possibility.
“I could have the anchor bust out of my femur, and it would be really painful. That’s something I have to watch for all the time,” he said.
Browning still has pain when standing for too long or sitting on a hard surface. The limited leg motion has made simple tasks more difficult, and even repositioning his leg while sleeping has been a challenge.
“I would hope that no one would have to go through what I’ve been through. There were a lot of things that could have gone better, and I wouldn’t be in this situation.”
But harder than the physical situation with his hip and the impact E. coli has had on his body is what it prevented him from being able to accomplish.
“I didn’t even get to finish boot camp, so they don’t even consider me a marine,” he said. “It’s very difficult not to have negative feelings. Given a chance, I would have worked for everything.”
Browning said he is thankful for his doctors and all they did to prevent the situation from becoming any worse, and for his family’s continued support. He will turn 22 in March and plans on attending college in the fall to study business. He also hopes to get a pilot license and dreams of teaching flying.
(To sign up for a free subscription to Food Safety News, click here)
]]>For those of you who read these fine pages of Food Safety News produced by Dan, Coral, Joe, Jonan, Cookson, and our many contributors on a daily basis for the past 10 years, I try not — well, at least not too often — to interject my legal side with my publisher side.
Here is an exception – Marler Clark needs help.
Well, more precisely, consumers of food around the world need help.
Since 2017 there been more than 500 people in the U.S. and Canada who have suffered E. coli O157:H7 illnesses linked to leafy greens grown in the U.S. Of these, nearly 200 have been hospitalized with 50 suffering hemolytic uremic syndrome (acute kidney failure known as HUS). There have been seven reported deaths.
Setting aside why outbreaks — no more romaining calm — are happening with frightening frequency and why so many of the illnesses seem so particularly brutal, the fact is that people, many children and the vulnerable, need legal advocacy.
So, here is my pitch: If you have been out of law school 2 to 5 years, send your cover letter, resume and writing sample to [email protected] or [email protected]. You must be willing to relocate to Seattle.
I am not looking for someone who wants just a job. I am looking for someone who is willing to think of this not as a job, but more of a calling. I want someone who will happily work beside some of the finest lawyers, doctors, nurses, epidemiologists, paralegals, experts and staff in the food safety business. We are dedicated to our clients 24/7/365 and I expect applicants to feel the same. This is NOT a 9 to 5 gig.
I recently was asked to write a Forward to a book on food safety for someone I greatly admire. I think if these words do not inspire you, you do not need to send an application.
Forward
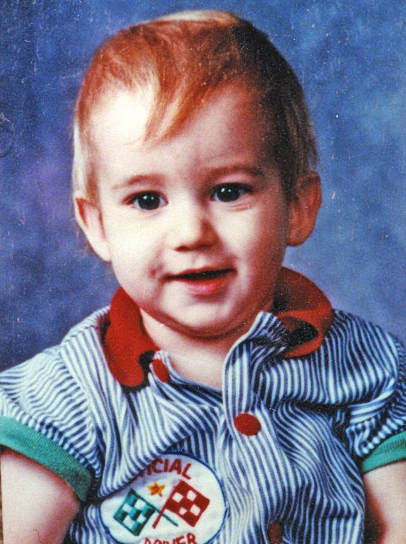
I never met Riley. However, I have a vivid memory after almost twenty-seven years of his tiny white casket flashing across the front page of the Seattle papers and the evening news. I remember the picture of Riley that Darin carries – a smiling toddler about to do mischief.
Riley’s life was a life cut short by a deadly pathogen that had been too long ignored by government and industry, and virtually unknown to consumers. In 1993 we all thought hamburgers were the all-American meal, not a recipe for death.
Riley and my daughter, Morgan, would have graduated from High School in 2010 and both been twenty-eight this year. For Darin, instead of twenty-eight years of memories and a future with a grown child, he has photos and videos of a forever young Riley and faded clippings of the public’s view of Riley’s agonizing death and the pain on his parent’s faces.
It is not without an anguished honor that I realize that the beginning of my life’s work is forever linked to Riley’s death and the deaths of Lauren Rudolph, Michael Nole and Celina Shribbs, and the devastating life-long illnesses of so many others caused by E. coli O157:H7, including Brianne Kiner, who was hospitalized for several months after Riley died a few hospital rooms away.
In the intervening years there have sadly been too many other Riley’s and Brianne’s. I have done what I could to help those families impacted by E. coli, Salmonella, Listeria and other foodborne pathogens. I have done what I could to change government and industry behavior by using the levers of the legal system. However, regardless how passionate I might be at times to be “put out of business,” it pales to what Darin Detwiler has done in the memory of his son.
As a lawyer, I have seen what can happen to a parent of a child that dies or has life-long complications caused be a pathogen like E. coli. Understandably, many never recover or simply cope by ignoring the pain. Few, like Darin, stare directly at the pain, embrace it, learn from it and teach us from it. Every word of this book written by Riley’s father carries a bit of Riley in every sentence, page and chapter. This book is important. Thank you Darin for writing it and thank you Riley for inspiring it.
No more to be said.
(To sign up for a free subscription to the morning news Food Safety News, click here.)
]]>





