Opinion
As of Nov. 9, 2021, health officials in Roanoke, Virginia, confirmed a total of 50 primary cases and two secondary cases of hepatitis A linked to a hepatitis A positive food service employee who worked at three Famous Anthony’s restaurants. Of those 52 cases, there have been at least 31 hospitalizations with one liver transplant, and unfortunately, three deaths.
Hepatitis A is a highly contagious disease that attacks the liver. It is also the only vaccine-preventable foodborne illness. Hepatitis A vaccines are available and given out nationwide for free by local health departments, or at a cost of less than $100.
So why aren’t all food workers vaccinated against hepatitis A? Your guess is as good as mine. According to the Centers for Disease Control and Prevention (CDC), hepatitis A vaccines are safe and effective at preventing hepatitis A infections. Severe allergic reactions following vaccination are rare, and the common side effects are usually mild and last 1-2 days.
Had the food service employee who exposed patrons of three Famous Anthony’s restaurants been vaccinated, the Seattle law firm Marler Clark would not be representing 27 individuals in this outbreak and the families of two who died. The cost to this restaurant will be in the tens of millions of dollars and will likely result in bankruptcy.
Here is what employers of food service employees and the CDC can do to prevent future illnesses, hospitalizations, and deaths.
Employer actions to prevent outbreaks of hepatitis A
Employers of food handlers can encourage their employees to get vaccinated and even mandate the hepatitis A vaccine.
Could employers face potential liability if any of their vaccinated employees has an adverse reaction to the vaccine?
Most of the talk on this topic is quite recent and related to the COVID-19 vaccine. But the laws relating to the COVID-19 vaccine are also likely applicable to other vaccines, including the hepatitis A vaccine.
An employer-mandated vaccine is considered a part of work, and thus, under most state laws, an adverse reaction would be covered by workers’ compensation. But, although injuries and illnesses from mandated vaccines are likely covered by the employer’s workers’ compensation policy, employers should check with their individual carriers.
When a vaccine is encouraged, but not mandated, however, coverage under workers’ compensation policies may not be available because any adverse reaction is unlikely to arise out of the employment. That does not necessarily mean that the employer would be held liable for any resulting injuries, however. According to the Society for Human Resource Management, “even if vaccination injury claims are not considered covered under workers’ compensation laws, an employee would need to demonstrate negligence on the part of the employer(.) . . . If FDA-approved vaccinations are administered by a third-party provider, it is difficult to see how a plaintiff would demonstrate such negligence.”
Furthermore, there are no-fault alternatives to the traditional tort system, such as the National Vaccine Injury Compensation Program, that provide compensation to people found to be injured by certain vaccines, including the hepatitis A vaccine.
What are the CDC’s recommendations on vaccinating food workers?
For years, CDC officials have said that food handlers did not need hepatitis A vaccinations because outbreaks are rare and food workers are not at increased risk of infection because of their jobs. They pointed to plummeting rates of hepatitis A infections since the introduction in 1996 of a safe and effective vaccine.
But CDC missed the point. Granted, food service workers are not more at risk of getting hepatitis A because of their occupation, but they are a risk for spreading it to customers. Moreover, although the incidence of hepatitis A has decreased, reported cases have increased dramatically since 2016, when large person-to-person outbreaks began occurring.
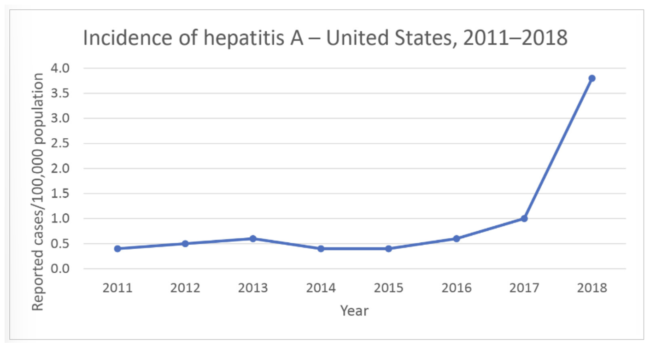
Source: CDC
It’s about time CDC changes its recommendations. Aside from the cost in human health and life, an outbreak of hepatitis A can be devastating for a food establishment in terms of liability and public relations. Just like healthcare workers need to be immunized against diseases they might encounter or transmit to their patients, food handlers need to be protected from being vectors of what can be a serious viral infection that is transmitted easily through food and drink.
(To sign up for a free subscription to Food Safety News, click here.)